Negative Thinking and Insomnia: Why Poor Sleep Creates Debbie Downer Syndrome

I lay awake at 3 AM again, thoughts spiraling through well-worn paths of worry. Tomorrow’s presentation, last week’s awkward conversation, and next month’s financial uncertainty—all amplified in the darkness. By morning, these midnight monsters had colored my entire outlook, and I carried that heaviness into my day. The worst part? I knew this destructive cycle would repeat when night fell again.
This painful dance between negative thinking and disrupted sleep isn’t just uncomfortable—it’s a self-reinforcing cycle that millions experience. The relationship runs more profound than most realize, with each condition not merely triggering but actively strengthening the other in a neurological feedback loop that can feel impossible to escape.
The Dangerous Dance: How Insomnia and Negative Thinking Feed Each Other
The connection between sleep and emotional regulation isn’t just a correlation—it’s a biological partnership that evolved over millennia. When this partnership falters, we experience what I’ve come to call “Debbie Downer Syndrome”—a state where poor sleep and negative thinking become locked in a mutually destructive embrace.
How Insomnia Breeds Negativity
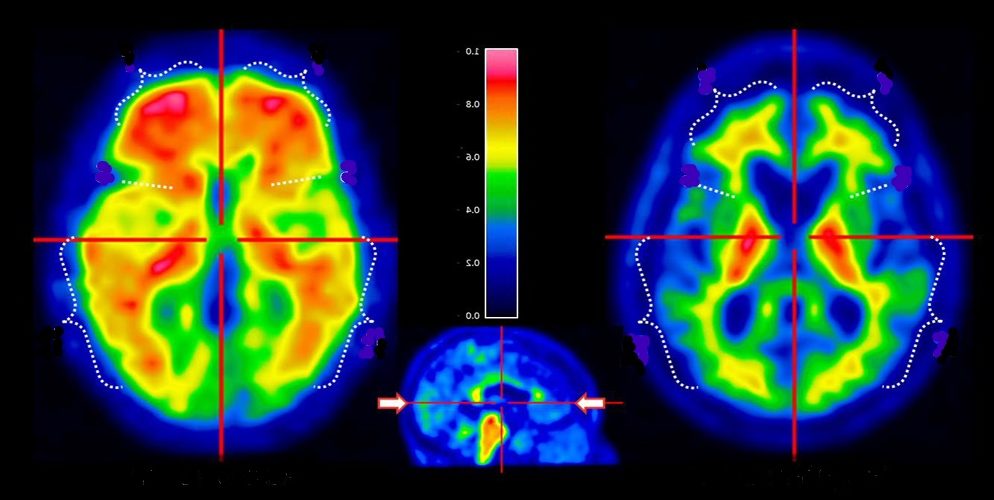
Sleep deprivation fundamentally alters how our brains process emotional information. Research from UC Berkeley revealed that inadequate sleep dramatically amplifies amygdala reactivity—our brain’s emotional processing center—while simultaneously reducing prefrontal cortex activity, which generally helps regulate those emotions.
This neurological imbalance creates a perfect storm:
Emotional filtering breaks down. Without sufficient sleep, our brain loses its ability to separate relevant threats from irrelevant ones. Your boss’s email becomes catastrophic; the slight tone change in your partner’s voice proves they’re falling out of love.
Negativity bias intensifies. Studies show sleep-deprived individuals show up to 60% stronger reactions to negative stimuli while demonstrating reduced ability to recall positive experiences. Your brain becomes a magnet for problems and blind to joys.
Stress reactivity increases. One night of poor sleep elevates cortisol levels by 15-20%, priming your entire system for heightened stress responses throughout the day.
Cognitive distortions flourish. Sleep disruption particularly impacts the brain regions responsible for rational thinking and perspective-taking. Without these cognitive brakes, catastrophizing, all-or-nothing thinking, and personalization run wild.
I experienced this firsthand during a project deadline that led to three consecutive nights of insufficient sleep. By day four, I found myself convinced colleagues were deliberately excluding me from conversations when, in reality, I had missed some emails while exhausted.
How Negative Thinking Destroys Sleep
The relationship works equally in reverse. Negative thought patterns actively sabotage sleep quality through multiple mechanisms:
Hyperarousal keeps the brain alert. Rumination—that endless replay of worries and problems—activates the sympathetic nervous system, flooding your body with sleep-inhibiting cortisol and adrenaline precisely when you need to relax.
Disrupted slow-wave sleep. Research using EEG measurements shows that negative thinking before bedtime reduces delta wave activity—the deep, restorative sleep stage most critical for emotional regulation and cognitive function.
Destructive sleep beliefs emerge. As insomnia persists, negative thoughts about sleep itself develop: “I’ll never sleep well again,” “Tomorrow is ruined because I can’t sleep,” or “Something is fundamentally wrong with me.” These beliefs create performance anxiety around sleep, making it even more elusive.
The circadian impact. Persistent negative thinking shifts gene expression related to circadian regulation, potentially altering your body’s fundamental sleep-wake timing system over time.
The Neurological Feedback Loop: How It Self-Perpetuates
This anomaly isn’t simply a matter of lousy sleep making you grumpy or anxious thoughts keeping you awake. Something far more insidious occurs at the neurological level—a genuine rewiring that strengthens this destructive partnership.
The default mode network (DMN)—brain regions active during self-referential thinking—becomes hyperconnected after sleep deprivation. This strengthened connectivity, such as negative self-focused rumination, makes interrupting more automatic and challenging.
Emotional memory consolidation shifts. During healthy sleep, our brains process emotional experiences, extracting lessons while dampening the raw emotional charge. Without adequate sleep, negative emotional memories retain their full painful potency, fueling future rumination cycles.
Neuroplasticity turns against us. The brain’s ability to form new neural pathways—usually positive—works against us here. Each night of rumination-disrupted sleep strengthens these pathways, making negative thinking and sleep disruption more automatic and resistant to change.
After three weeks of poor sleep during a particularly stressful period, I noticed my thought patterns had changed even during calm moments. My brain would automatically generate worst-case scenarios for inconsequential circumstances. It wasn’t just bad moods anymore—my neural pathways had been reinforced toward negativity.
The Wider Impact: Beyond Bad Moods
The personal and relationship consequences extend far beyond feeling grumpy or tired:
Cognitive performance declines. After two consecutive nights of poor sleep, one’s working memory drops by 40%. Problem-solving abilities, creative thinking, and decision-making deteriorate, reinforcing negative self-appraisal.
Emotional resilience crumbles. The ability to bounce back from setbacks—a key component of mental health—diminishes dramatically with ongoing sleep disruption.
Physical health suffers. Immune function decreases by up to 70% during periods of insomnia, while inflammation markers rise, creating vulnerability to both illness and pain that further feeds negative thinking.
Relationship damage accumulates. Sleep-deprived individuals show reduced empathy, increased irritability, and poorer communication skills—straining the very support systems that could help break the cycle.
Sleep Recovery: Breaking the Cycle Without Years of Therapy
The good news is that this frustrating feedback loop can be interrupted relatively quickly when approached strategically. Sleep recovery techniques offer a powerful entry point that addresses both conditions simultaneously without requiring extended therapy.
Strategic Sleep Interventions That Reset Negative Thinking
Cognitive Shuffling disrupts rumination through deliberate mental redirection. Rather than fighting negative thoughts directly, this technique has you generate random, non-emotional words beginning with the same letter (A: apple, airplane, antelope…). This simple cognitive task interrupts the DMN’s rumination circuits while providing enough mental engagement to ease sleep onset.
I discovered this accidentally while playing word games during a bout of insomnia. Within a week of intentional practice, my sleep onset time and morning mood had improved noticeably.
Paradoxical Intention tackles sleep performance anxiety by temporarily removing the pressure to sleep. By intentionally staying awake (while remaining restful), you short-circuit the performance anxiety that often accompanies chronic insomnia. Studies show this reduces sleep onset time and the catastrophic thinking that emerges around sleep difficulties.
Stimulus Control helps recondition your bedroom as a place of rest rather than rumination. By using your bed exclusively for sleep and leaving the environment when unable to sleep after 20 minutes, you break the environmental triggers for insomnia and negative thinking loops.
Cognitive Recalibration Techniques That Improve Sleep Quality
Constructive Worry Practice creates a dedicated 15-minute worry session well before bedtime. Writing down concerns and initial action steps earlier in the evening has been shown to reduce pre-sleep rumination by up to 73% in studies while improving sleep efficiency.
Cognitive Defusion techniques create psychological distance from negative thoughts. Rather than fighting or believing troubling thoughts, you learn to observe them as mental events: “I notice I have the thought that I’ll fail tomorrow” rather than “I’m going to fail tomorrow.” This subtle shift reduces the emotional charge that disrupts sleep onset.
Self-compassion practices directly counter the harsh self-criticism that often accompanies insomnia and negative thinking. Brief self-compassion exercises before bed have been shown to improve sleep quality and next-day emotional regulation—a double benefit for breaking the cycle.
Physical Approaches With Cognitive Benefits
Strategic Light Exposure helps reset circadian rhythms while improving mood regulation. Morning bright light exposure for 15-30 minutes increases serotonin production, improves nighttime melatonin release, and directly impacts regions involved in cognitive-emotional processing.
Core Temperature Regulation through a warm bath or shower 1-2 hours before bedtime triggers natural sleepiness while simultaneously reducing muscle tension, contributing to negative rumination.
The Recovery Timeline: Realistic Expectations
Unlike some therapeutic approaches that may require months or years, targeted sleep recovery can break the negative thinking-insomnia cycle relatively quickly:
Days 1-3: Initial improvement in either sleep or thinking (rarely both immediately). Days 4-7: Noticeable reduction in daytime rumination and improvement in sleep onset. Weeks 2-3: Significant improvement in both conditions, with established new patterns. Months 1-3: Consolidation of improvements and increased resilience against relapse
Frequently Asked Questions
Is it better to target negative thinking or insomnia first?
For most people, focusing on sleep behaviors creates the quickest route to improvement in both conditions. Sleep improvement enhances cognitive processing and emotional regulation, building a foundation for effective thought management. However, if catastrophic thoughts about sleep are your primary issue, beginning with gentle cognitive techniques may be preferable.
Can medications help break the cycle?
While sleep medications can provide temporary relief, research shows they generally don’t address the underlying relationship between negative thinking and sleep disruption. Most sleep medications suppress REM sleep—the stage critical for emotional processing. Short-term medication use combined with behavioral approaches may help in severe cases, but behavioral and cognitive techniques create more sustainable improvements.
How do I know if my negative thinking is causing my insomnia or vice versa?
Try this self-assessment: Do negative thoughts primarily emerge during the day and continue into bedtime? Or do you generally think more positively during the day, with negativity emerging primarily during nighttime wakefulness? The former suggests negative thinking as the primary driver; the latter points to insomnia as the initial trigger. However, after several weeks, the cycle becomes so intertwined that addressing both conditions simultaneously is most effective.
What if I improve my sleep but still experience negative thinking?
Some individuals find that while sleep improves, negative thinking patterns persist due to their automated nature. Adding more structured cognitive approaches like Cognitive Behavioral Therapy may be beneficial in these cases. However, many report consistent and restful sleep substantially improves their resilience against negative thinking, even without direct cognitive intervention.
Remember that breaking this cycle isn’t about achieving perfect sleep or eternally positive thinking. It’s about interrupting destructive relationships enough to restore your natural resilience and balance. Sometimes, a good night’s sleep can be the first step toward restoring your emotional well-being from this challenging cycle.