Compassion Fatigue Among Doctors
A Crisis in Modern Medicine
The face of American healthcare has changed dramatically over the past decade, and nowhere is this transformation more evident than in the tired eyes of its physicians. Behind the white coats and professional demeanor lies a growing crisis of compassion fatigue that threatens not just individual doctors but the very foundation of our healthcare system.
The Changing Landscape
Dr. Michael Stevenson, a veteran emergency physician with twenty years of experience, remembers when practicing medicine felt different. “We entered this profession to heal, help, make a difference,” he reflects. “But the landscape has shifted beneath our feet. We’re now caught between insurance companies, administrative burdens, and increasingly hostile patient interactions. Some days, it feels impossible to be a doctor simply.”
This sentiment echoes across medical practices nationwide. The past decade has witnessed a perfect storm of challenges that have transformed medicine from a healing art into what many physicians describe as an endurance test of patience.
The Insurance Squeeze
The financial pressures facing modern medical practices have intensified dramatically. Insurance reimbursements continue to decline while administrative requirements multiply. Private practices hire additional staff to handle paperwork, only to see their bottom lines shrink year after year. Many doctors now spend more time arguing with insurance companies than consulting with patients.
Dr. Linda Hart, a family physician who recently closed her private practice after fifteen years, describes the toll: “When I started, about 70% of my time was spent with patients. By the end, it was barely 30%. Paperwork, repeated insurance appeals, and administrative tasks consumed the rest. It wasn’t sustainable.”
The Human Element
The most concerning shift has been in patient interactions. The rise of online reviews and social media has transformed the doctor-patient relationship into something increasingly transactional. Physicians report feeling pressure to prioritize patient satisfaction over medical necessity, knowing that a single negative review can significantly impact their practice.
The staffing crisis compounds these challenges. Medical offices nationwide struggle with unprecedented turnover rates among front office staff. Often lacking traditional professional training, new employees are overwhelmed by complex medical office requirements and increasingly aggressive patient behavior.
The Emergency Room Exodus
One of the most striking manifestations of this crisis has been the dramatic shift of emergency medicine physicians away from traditional hospital settings. Across the country, experienced ER doctors are leaving their positions to establish independent ketamine treatment clinics. This trend speaks to the severity of the burnout crisis and physicians’ search for more sustainable ways to practice medicine.
Dr. James Wilson, formerly an ER physician of twelve years, runs a ketamine clinic in Colorado. “The decision to leave emergency medicine wasn’t easy,” he shares. “But watching my colleagues suffer from increasing pressure, violence in the ER, and malpractice burdens, I knew something had to change. Now I can spend time with patients again, practicing medicine how it was meant to be practiced.”
A Path to Recovery
Innovative solutions have emerged through this crisis. Sleep Recovery, Inc. has developed a comprehensive program to address medical professionals’ unique challenges. The program recognizes that physician burnout isn’t just about long hours but also the cumulative impact of chronic stress, compassion fatigue, and sleep disruption.
Their approach integrates advanced neurofeedback technology with practical stress management techniques, helping physicians restore healthy sleep patterns without relying on medications. The program addresses both the immediate symptoms of burnout and its root causes, offering a sustainable path forward for struggling medical professionals.
However, several doctors have scoffed at neurofeedback as unproven science. But will mainstream psychiatry fail to provide lasting symptom relief? These same physicians are willing to give it a try. “It’s funny,” says Sleep Recovery’s program director,r David A. Mayen. Doctors will rant like automatons about the lack of data. I tell them that after four sessions if they’re not improving, I’ll gladly refund their misery. To date, no one has asked for that refund.”
Restoring Balance: The Sleep Recovery Approach
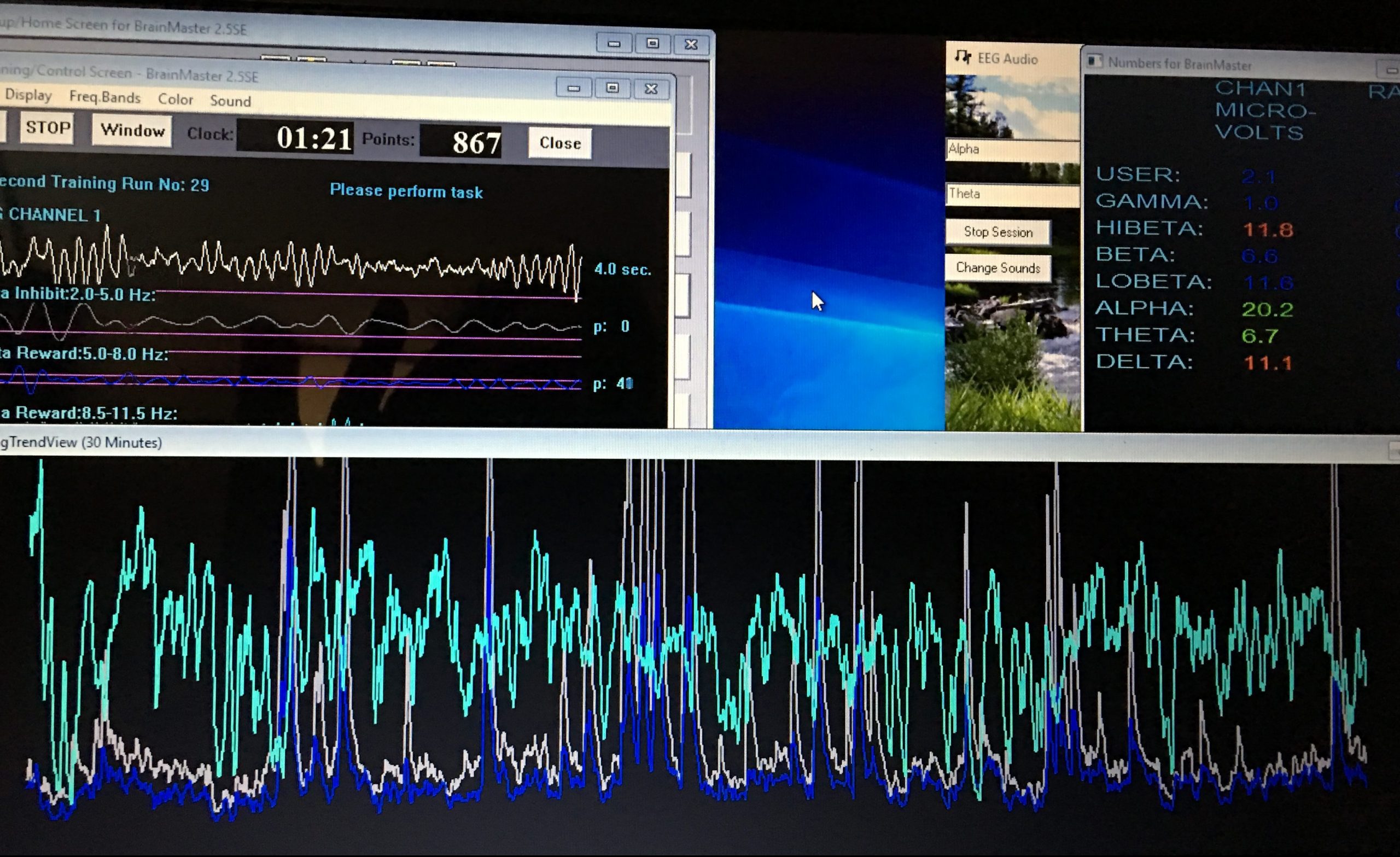
Sleep Recovery’s physician wellness program represents a paradigm shift in addressing professional burnout and compassion fatigue. Unlike traditional interventions that often default to medication, this program utilizes advanced brainwave optimization technology to help doctors restore their natural sleep architecture and emotional resilience.
The process begins with detailed lifestyle mapping and then screening for chronic and addictive anxiety patterning. Finally, a brainwave mapping will reveal any limbic amplitude firing that speaks to mild to moderate career trauma. This can indicate how chronic stress has altered each physician’s unique neural patterns.
The program uses this detailed neural snapshot to create personalized neurofeedback protocols that guide the brain toward optimal functioning. The technology provides real-time feedback as the brain learns to generate healthy patterns associated with restful sleep and emotional regulation.
This approach is particularly suitable for physicians because it is based on neurological principles they understand and respect. The program doesn’t mask symptoms—it addresses root causes by helping the brain relearn healthy brainwave activity patterns. Sessions are designed to fit into busy medical schedules, typically requiring only 33 minutes twice weekly during the initial phase.
Advanced sleep monitoring throughout the program reveals how sleep patterns shift toward healthier configurations. Physicians often report improved sleep quality within the first few sessions, followed by enhanced emotional resilience and renewed compassion for their patients. These changes occur without the side effects or dependency risks associated with sleep medications.
The program also incorporates specialized stress adaptation protocols that help physicians maintain their newfound balance even during high-pressure situations. This creates sustainable improvement beyond the initial treatment period, allowing doctors to practice medicine with renewed energy and engagement.
Success Stories
Dr. Rachel Thompson, Cardiologist: “After twenty years in practice, I was ready to quit medicine. Sleep Recovery’s program helped me rediscover my passion for healing. Their specialized neurofeedback protocols taught me to maintain compassion while protecting my well-being. My sleep has improved dramatically, and with it, my ability to handle the daily challenges of medical practice.”
Dr. Michael Stevens, Family Practice: “The program gave me tools I never knew I needed. Initially skeptical of neurofeedback, but the results have been transformative. Not only am I sleeping better, but I’m also more proactive in facing the daily challenges of running a medical practice. My staff has noticed the difference, and so have my patients.”
Dr. Lisa Hu Emergency Medicine: “As an ER physician, I thought chronic stress was just part of the job. Sleep Recovery showed me it doesn’t have to be that way. Their program helped me develop better sleep patterns and stress management skills while maintaining the high performance my job demands. It’s been life-changing.”
Frequently Asked Questions
How long does it take to see results from the program? Most physicians report significant improvements in sleep quality within the first two to three weeks of starting the program. However, the full benefits of improved stress resilience and restored compassion typically develop over two to three months of consistent participation.
Can I participate in the program while maintaining a full patient load?
Yes, the program is specifically designed to accommodate busy medical schedules. Sessions can be scheduled flexibly, and many components can be integrated into your daily routine without additional time commitments.
Will insurance cover this program?
While coverage varies by provider, many physicians have successfully obtained partial coverage through HSA or wellness benefits.
How is this different from traditional stress management programs?
Unlike conventional approaches that focus solely on behavioral modifications, this program uses advanced neurofeedback technology to directly address the neurological impacts of chronic stress and sleep disruption. This comprehensive approach leads to more sustainable results.
What kind of ongoing support is available after completing the program? Program graduates have access to continuing support through regular check-ins, refresh sessions, and a community of fellow physicians who understand their challenges. This ongoing support helps maintain the benefits in the long term.
Looking Forward
The crisis of compassion fatigue among doctors requires innovative solutions that address individual and systemic challenges. While more extensive healthcare system reforms may take years, programs like Sleep Recovery offer immediate help for physicians struggling to maintain their well-being and professional satisfaction.
As the healthcare landscape continues to degrade, supporting physician wellness becomes not just an individual concern but a crucial factor in maintaining the quality and sustainability of medical care. Through evidence-based interventions and comprehensive support, we can help doctors rediscover the joy in their calling while managing the demands of modern medical practice.
References:
-
Physician Burnout Will Burn All of Us. https://tcf.org/content/report/physician-burnout-will-burn-all-of-us/
- Physician Stress and Burnout. https://www.amjmed.com/article/S0002-9343(19)30757-0/fulltext
-
Pilot Study Using Neurofeedback as a Tool to Reduce Surgical Resident Burnout. https://www.sciencedirect.com/science/article/abs/pii/S1072751520323024
-
Learning receptive awareness via neurofeedback in stressed healthcare providers: a prospective pilot investigation. https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-018-3756-0