Can TMJ Cause Sleep Problems?
Understanding the Complex Connection
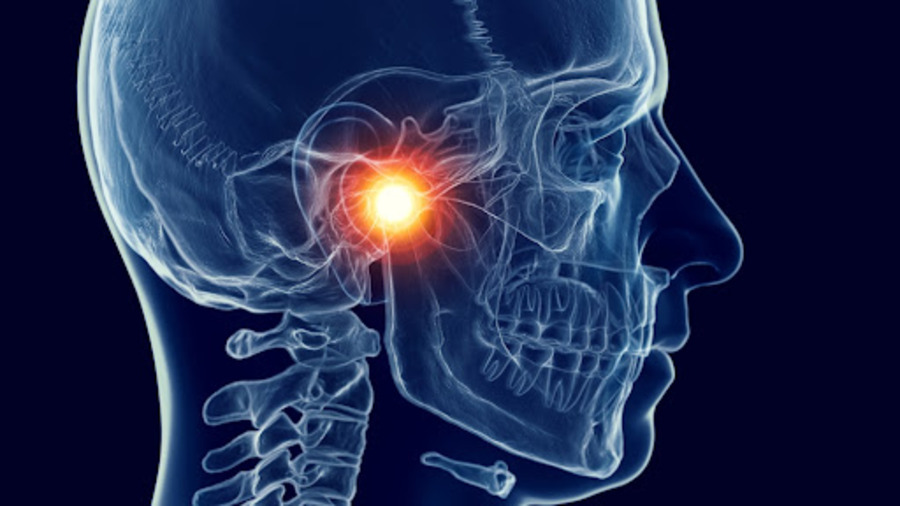
The interconnectivity between temporomandibular joint (TMJ) dysfunction and sleep disturbance reveals a fascinating physical, emotional, and neurological health intersection. While many view TMJ as simply a jaw problem, research shows that it is a complex condition that can profoundly impact sleep and emotional well-being.
Understanding TMJ: Beyond the Joint
The temporomandibular joint’s story begins deep in our evolutionary history. In 1934, Dr. William Costen, an otolaryngologist, first documented the constellation of symptoms we now associate with TMJ dysfunction. However, archaeological evidence suggests humans have struggled with this condition for thousands of years, with ancient Egyptian and Roman texts describing similar symptoms.
Recent research at the University of Michigan’s Sleep Disorders Center reveals that TMJ dysfunction affects approximately 12% of the population at any given time, with women being affected at nearly twice the rate of men. This gender disparity hints at hormonal and stress-related factors that extend far beyond simple mechanical issues.
The Pain-Sleep-Anxiety Cycle
The relationship between TMJ and sleep disruption often creates a self-perpetuating cycle. Dr. William George Brose’s research at Stanford’s Pain Management Center demonstrates how TMJ pain can:
- Prevent the initiation of deep sleep
- Cause frequent sleep interruptions
- This leads to chronic sleep debt
- Exacerbate anxiety and depression
This cycle becomes particularly vicious because poor sleep increases pain sensitivity, leading to more TMJ discomfort, which further disrupts sleep.
The Emotional Component
- Recent research has uncovered strong connections between TMJ dysfunction and emotional trauma. Dr. Taylor Burke’s groundbreaking study at The Mood and Behavior Lab reveals that individuals with unresolved trauma show significantly higher rates of TMJ problems. This connection appears to operate through several mechanisms:
The Trauma Connection
Emotional trauma can manifest physically through:
- Increased muscle tension in the jaw and neck
- Altered pain processing pathways
- Disrupted stress hormone regulation
- Modified neural pain thresholds
The Anxiety Factor
Longitudinal studies show that individuals with diagnosed anxiety disorders are three times more likely to develop TMJ symptoms within five years.
Manifestation Patterns
The anxiety-TMJ connection typically follows several patterns:
- Nocturnal bruxism (teeth grinding)
- Daytime jaw clenching
- Muscle tension headaches
- Sleep onset difficulties
The Sleep Disruption Cascade
The impact of TMJ on sleep architecture proves particularly fascinating. Studies reveal that TMJ sufferers experience:
- Reduced deep sleep periods
- Increased sleep fragmentation
- Altered REM sleep patterns
- Compromised sleep efficiency
The Neurofeedback Solution: Sleep Recovery’s Approach
The Sleep Recovery Program’s approach to TMJ-related sleep disruption represents a paradigm shift in treatment. Rather than focusing solely on mechanical interventions, this program addresses the underlying neurological patterns that perpetuate the TMJ-sleep-anxiety cycle.
Neural Retraining
Using advanced neurofeedback techniques, the program helps stabilize irregular brainwave patterns commonly seen in TMJ sufferers.
This process works through several mechanisms:
First, the program identifies specific brainwave patterns associated with chronic pain and anxiety. These patterns often show excessive high-frequency activity and reduced alpha wave presence – a signature commonly seen in chronic pain conditions.
Patients learn to regulate these patterns through targeted feedback protocols, gradually shifting their nervous system toward a more balanced state. This regulation often leads to:
- Reduced muscle tension
- Improved pain tolerance
- Enhanced sleep initiation
- Better emotional regulation
The Recovery Process
The Sleep Recovery Program typically observes several phases of improvement:
Initial Phase (Weeks 1-2): Patients often report reduced anxiety and muscle tension, with many experiencing improved sleep onset.
Intermediate Phase (Weeks 3-4): Sleep architecture begins to normalize, with increased periods of deep sleep and reduced nocturnal bruxism.
Advanced Phase (Months 5-6): Many patients report significant reductions in TMJ symptoms, sleep disruption, and improved emotional resilience.
Advanced Research Insights
Recent studies using advanced imaging techniques have revealed fascinating connections between TMJ dysfunction and broader neurological patterns. Dr. Patricia Hammond’s research at the Mayo Clinic’s Neurology Department has identified specific neural signature patterns in TMJ sufferers that differ markedly from those without the condition.
Neural Imaging Revelations
Using combined fMRI and EEG monitoring, Dr. Hammond’s team discovered that TMJ patients show:
- Altered activity in the anterior cingulate cortex
- Modified pain processing in the thalamus
- Disrupted connectivity in the default mode network
- Enhanced activity in anxiety-related brain regions
These findings suggest that TMJ isn’t just a local joint condition but a complex neurological phenomenon that simultaneously affects multiple brain systems.
Gender-Specific Patterns
Female patients often experience cyclical variations in TMJ symptoms that correlate with hormonal changes. This pattern suggests complex interactions between:
- Reproductive hormones
- Stress response systems
- Pain processing networks
- Sleep regulation mechanisms
Impact on Daily Function
Cognitive Effects
- Reduced working memory capacity
- Impaired decision-making abilities
- Decreased attention span
- Compromised emotional regulation
Professional Impact
- Increased workplace errors
- Reduced productivity
- Compromised communication abilities
- Higher rates of sick leave
The Social Dimension
Relationship Strain
- Partner sleep disruption
- Communication difficulties
- Reduced social engagement
- Emotional distance
Family Dynamics
- Parenting challenges
- Household tension
- Modified family routines
- Caregiver burden
Novel Treatment Approaches
Beyond traditional interventions, several innovative treatment modalities have shown promise in addressing TMJ-related sleep disruption:
Mindfulness-Based Interventions
- Reduce muscle tension
- Lower anxiety levels
- Improve sleep quality
- Enhance pain management
Chronotherapy Applications
Emerging research in chronobiology suggests that timing-based interventions can significantly impact TMJ symptom management:
- Strategic light exposure
- Meal timing optimization
- Activity scheduling
- Sleep phase alignment
Genetic Factors
Recent genetic studies have unveiled hereditary components:
- Connective tissue strength
- Pain sensitivity thresholds
- Stress response patterns
- Neural inflammation tendencies
Long-Term Prognosis
Longitudinal studies reveal varying outcomes based on treatment approach and individual factors:
Key Prognostic Indicators
- Early intervention timing
- Comprehensive treatment adoption
- Lifestyle modification success
- Support system strength
Recovery Trajectories
Patient outcomes typically fall into several categories:
- Rapid responders (30%)
- Gradual improvers (45%)
- Chronic manageable (20%)
- Treatment-resistant (5%)
Looking Forward
The understanding of TMJ’s relationship with sleep continues to evolve. Recent research suggests that addressing the condition requires a comprehensive approach that considers the following:
- Neurological factors
- Emotional components
- Sleep architecture
- Stress management
Current and Future Treatments
The success of neurofeedback-based approaches in treating TMJ-related sleep disruption offers hope for those caught in the pain-sleep-anxiety cycle. These programs provide a path toward sustainable recovery by addressing the condition’s root causes rather than just its symptoms.
Conclusion
The connection between TMJ, sleep problems, and emotional wellbeing represents a complex interplay of physical and psychological factors. Understanding this relationship helps explain why traditional treatments focusing solely on mechanical aspects often provide incomplete relief.
References:
- Association between temporomandibular disorders and anxiety: A systematic review. https://pmc.ncbi.nlm.nih.gov/articles/PMC9606663/
-
Psychoimmunology, anxiety disorders and TMJ-disorders. https://link.springer.com/chapter/10.1007/978-3-7091-6870-7_10
-
Temporomandibular joint disorders contribute to anxiety in BalB/C mice. https://www.sciencedirect.com/science/article/abs/pii/S0006291X19311763
- Association between Sleep Disorders and Sleep Quality in Patients with Temporomandibular Joint Osteoarthritis: A Systematic Review. https://pmc.ncbi.nlm.nih.gov/articles/PMC9495859/
-
Quality of life, chronic pain, insomnia, and jaw malfunction in patients after alloplastic temporomandibular joint replacement: a questionnaire-based pilot study. https://www.sciencedirect.com/science/article/pii/S090150272030374X
