Psychiatric Illness and Sleep: How Insomnia Connects Psychiatric Disorders to Dementia Risk

New research reveals that people with multiple psychiatric disorders face dramatically higher dementia risk, with odds increasing up to 11 times normal. Sleep recovery expert Jefferey Wilson, PhD, believes the missing piece of this puzzle is chronic sleep disruption – the hidden thread connecting mental health struggles to cognitive decline.
A groundbreaking study published in BMJ Mental Health has sent shockwaves through the medical community. Researchers analyzing nearly 4,000 patients found something alarming: people with multiple psychiatric disorders don’t just face higher dementia risk – they face catastrophically higher risk.
The numbers tell a stark story. Having two psychiatric conditions doubles your dementia odds. Three conditions increase risk by 4.6 times. But four or more psychiatric disorders? Your dementia risk shoots up 11 times higher than that of someone with a single condition.
Most troubling of all, people with both mood and anxiety disorders showed dementia probabilities reaching nearly 90% in some cases.
These findings raise urgent questions about what connects psychiatric struggles to cognitive decline. While mainstream researchers debate data about systemic inflammation and blood-brain barrier dysfunction, the contrarian cohort believes the answer lies in something simpler yet profound: sleep.
The Sleep Recovery Perspective
Dr. Jefferey Wilson, clinical director of Sleep Recovery, Inc., has spent over 15 years studying the intricate relationships between sleep, mental health, and cognitive function. His perspective offers a unifying theory that could explain the dramatic dementia risks revealed in the BMJ study.
“What we’re seeing in this research isn’t surprising when you understand sleep’s role,” Wilson explains. “Poor sleep quality over extended periods creates a cascade of problems that manifest as psychiatric disorders first, then progress to cognitive decline and eventually dementia.”
Dr. Wilson’s theory challenges the traditional view that treats psychiatric disorders and dementia as separate medical issues. Instead, he sees them as different stages of the same underlying problem: chronic sleep disruption that gradually erodes brain function over time.
This perspective emerged from years of working with clients whose psychiatric symptoms dramatically improved once their sleep patterns were restored. Time and again, he observed that addressing sleep problems didn’t just improve mood and anxiety – it often prevented or reversed early cognitive decline.
The French Study: A Wake-Up Call
The BMJ Mental Health study, conducted by researchers at Bicêtre Hospital in France, tracked 3,688 patients over 14 years. The results paint a concerning picture of how psychiatric disorders compound dementia risk.
Among the most striking findings: patients with both mental disorders (like clinical depression or substance abuse disorder) and anxiety disorders showed dementia probabilities ranging from 48% to nearly 90%. This peer-reviewed study wasn’t a small sample – the pattern held across hundreds of patients with these combined conditions.
The study’s lead researchers noted the “dose-response” relationship between psychiatric disorders and dementia risk. Each additional psychiatric condition didn’t just add to dementia risk – it multiplied it exponentially.
Dr. Antoine Edel, one of the study authors, observed that the short time between psychiatric diagnoses and dementia onset (averaging just 1.6 years) suggests these mental health conditions might be early warning signs of impending cognitive decline.
The Sleep Connection: More Than Correlation
While the French researchers propose several theories for their findings – including brain inflammation and medication effects – Wilson believes they’re missing the fundamental driver: sleep disruption.
“Every psychiatric disorder we know of involves sleep problems,” he points out. “Depression disrupts sleep architecture. Anxiety creates hypervigilance that prevents deep sleep. Bipolar disorder often begins with severe sleep disruption during manic episodes. The pattern is consistent across all mental health conditions.”
This observation aligns with decades of sleep research showing that chronic sleep problems don’t just accompany psychiatric disorders – they often precede them. Studies following healthy individuals over time consistently find that sleep problems emerge months or years before psychiatric symptoms become apparent.
But Wilson goes further, arguing that the same sleep disruption that contributes to psychiatric disorders also sets the dementia stage. The brain’s nightly maintenance processes – including the clearance of toxic proteins associated with Alzheimer’s disease – depend on specific sleep stages that become impaired in chronic insomnia.
The Brain’s Nightly Maintenance System
During healthy sleep, the brain undergoes crucial maintenance processes that prevent both psychiatric symptoms and cognitive decline. The glymphatic system, discovered relatively recently, acts like the brain’s garbage disposal, clearing out cellular waste, including amyloid and tau proteins associated with Alzheimer’s disease.
This system operates primarily during deep sleep stages. When sleep becomes fragmented or insufficient, toxic proteins accumulate. Over time, this accumulation contributes to both the inflammation seen in psychiatric disorders and the neural damage characteristic of dementia.
“Think of it like not taking out the trash for months,” Wilson explains. “Eventually, the buildup creates problems throughout the house. In the brain, that buildup manifests as mood problems first, then memory problems, and eventually full-blown dementia.”
Research supports this model. Studies using brain imaging have shown that even one night of sleep deprivation increases amyloid accumulation in brain regions affected by Alzheimer’s disease. Chronic sleep problems accelerate this process dramatically.
Sleep Problems May Lead to Psychiatric Disorders
The BMJ study’s finding that multiple psychiatric disorders dramatically increase dementia risk makes perfect sense through a sleep lens. Sleep disruption affects numerous brain systems, creating causation for various psychiatric conditions.
The prefrontal cortex, which regulates emotions and executive function, is particularly sensitive to sleep loss. When this brain region becomes impaired, people develop symptoms that might be diagnosed as depression, anxiety, or attention problems – sometimes all three.
Sleep problems also disrupt the body’s stress response system, leading to chronic inflammation that affects brain function. This recursive loop creates a vicious cycle where sleep problems worsen psychiatric symptoms, which in turn make sleep even more difficult.
Over time, this compound stress on brain systems creates the “multiple psychiatric disorder” pattern seen in the French study. But rather than separate conditions, Mayen sees these as different manifestations of the same underlying sleep-related brain dysfunction.
“We often see clients diagnosed with depression, anxiety, and attention problems,” he notes. “But when we restore their sleep, all these symptoms improve together. That’s because they stem from the same source – sleep-deprived brain circuits that can’t function properly.”
The Progression to Dementia
As sleep problems persist over years or decades, the brain’s ability to maintain itself deteriorates further. The same processes that initially created psychiatric symptoms eventually lead to more severe cognitive impairment.
The BMJ study’s finding that mood and anxiety disorders together create the highest dementia risk makes biological sense. Both conditions involve chronic activation of stress systems that disrupt sleep quality. When co-occurring, they create a “perfect storm” of sleep disruption that overwhelms the brain’s maintenance capacity.
This new data explains why the French researchers found such short intervals between psychiatric diagnoses and dementia onset. By the time multiple psychiatric conditions are diagnosed, the underlying sleep-related brain dysfunction may be pretty advanced.
Mayen believes this progression isn’t inevitable. “If we can restore healthy sleep patterns before permanent damage occurs, we can often reverse the trajectory. But the window for intervention gets smaller as more psychiatric symptoms accumulate.”
Sleep Recovery’s Comprehensive Approach
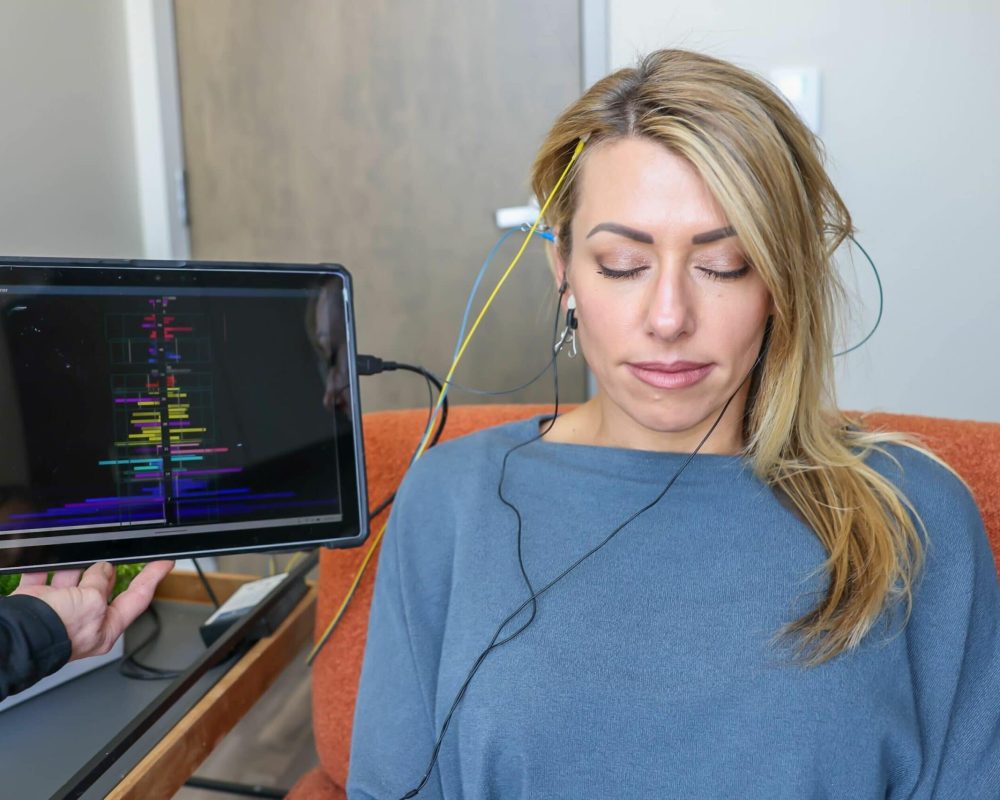
Sleep Recovery’s program, developed over 15 years of clinical experience, addresses the sleep disruption that Wilson believes underlies both psychiatric disorders and dementia risk. The approach uses FDA-approved brainwave entrainment technology to retrain dysfunctional sleep patterns.
The program’s core rests on understanding that chronic insomnia isn’t just about difficulty falling asleep – it’s about disrupted brain wave patterns that prevent proper sleep architecture. Using precise EEG training frequencies, the technology guides the brain back to healthy sleep patterns that support both mental health and cognitive function.
“We’re not precisely treating insomnia,” he explains. “We’re addressing the neurological dysfunction that manifests as sleep problems, psychiatric symptoms, and eventually cognitive decline.”
The 30-minute sessions, conducted every other day, work by entraining brain waves to frequencies associated with healthy sleep stages. In time, the client’s brain learns to maintain these patterns autonomously, restoring the natural sleep architecture needed for mental and cognitive health.
Sleep Recovery’s results align with their theory about sleep’s central role in psychiatric and cognitive health. Clients typically achieve (although results may vary) 6.5 to 8.5 hours of quality sleep per night within weeks of beginning the program. More importantly, they often experience an 85% reduction in anxiety levels and significant improvements in mood disorders.
But relevant to the BMJ study, many clients report gains in cognitive function – better memory, clearer thinking, and improved focus. These cognitive gains often occur alongside mental health improvements, supporting the idea that both may stem from restored sleep function.
“We regularly see clients in their 60s and 70s whose memory problems improve dramatically once their sleep is restored,” Mayen reports. “This suggests that at least some of what we label as early dementia might actually be reversible sleep-related cognitive impairment.”
This observation has profound implications for the millions of older adults experiencing both sleep problems and early cognitive changes. Rather than accepting these as inevitable aspects of aging, Mayen’s approach suggests they might be treatable manifestations of sleep dysfunction.
The Inflammation Connection
The BMJ study’s authors proposed that inflammation might explain the link between psychiatric disorders and dementia. This theory aligns perfectly with sleep research showing that chronic sleep disruption triggers inflammatory processes throughout the body and brain.
Sleep loss activates the immune system in ways that promote chronic inflammation. This inflammatory state contributes to both psychiatric symptoms and the neural damage seen in dementia. Studies have found elevated inflammatory markers in people with depression, anxiety, and early Alzheimer’s disease.
By restoring healthy sleep patterns, Sleep Recovery’s approach may interrupt this inflammatory cascade before it causes permanent damage. Research shows that even modest improvements in sleep quality can reduce inflammatory markers and improve both mood and cognitive function.
“When you fix the sleep problem, you often fix the inflammation problem,” Wilson observes. “And when inflammation decreases, both psychiatric symptoms and cognitive problems tend to improve.”
Medication Complications
The French study noted that accumulating psychiatric medications might contribute to increased dementia risk. This observation resonates with Dr. Wilson’s experience, as many Sleep Recovery clients are taking multiple psychiatric medications when they begin the program.
Common psychiatric medications – including benzodiazepines, certain antidepressants, and antipsychotics – can actually worsen sleep quality despite their sedating effects, creating a paradox where medicines prescribed to treat psychiatric symptoms may perpetuate the sleep dysfunction underlying those symptoms.
Benzodiazepines, commonly prescribed for anxiety, are particularly problematic. Recent research has shown these medications disrupt the brain’s natural sleep architecture and may accelerate cognitive decline through mechanisms involving mitochondrial dysfunction.
“We often see clients who are taking multiple medications but still can’t sleep properly. The medications might help with immediate symptoms, but they’re not addressing the underlying sleep dysfunction. Sometimes they’re making it worse.”
As clients’ sleep improves through the Sleep Recovery program, many can reduce or eliminate psychiatric medications under they’re prescribing physician’s supervision. This medication reduction often leads to further improvements in sleep quality and cognitive function.
The Cardiovascular Link
The BMJ study controlled for cardiovascular risk factors, but these conditions share essential connections with both sleep and dementia risk. Sleep problems contribute to hypertension, diabetes, and heart disease – all established dementia risk factors.
Sleep Recovery’s approach may provide cardiovascular benefits alongside mental health improvements. Research shows that restoring healthy sleep patterns can reduce blood pressure, improve glucose metabolism, and decrease inflammation – all factors that protect against both psychiatric disorders and dementia.
“When people start sleeping better, their whole physiology improves, blood pressure comes down, mood stabilizes, and thinking becomes clearer. It’s all connected through simple sleep quality.”
This holistic improvement may explain why addressing sleep problems can have such dramatic effects on overall health and function. Rather than treating individual symptoms, the approach targets a fundamental process that affects multiple body systems.
The BMJ study’s findings suggest that multiple psychiatric disorders might serve as early warning signs of dementia risk. From Wilson’s perspective, the real warning sign is the sleep disruption that underlies these psychiatric conditions.
Recognizing sleep problems as potential harbingers of both mental health and cognitive issues opens new possibilities for prevention. Rather than waiting for psychiatric symptoms to develop and worsen, early intervention focused on sleep could prevent the cascade toward dementia.
Key warning signs include difficulty falling asleep, frequent night wakings, early morning awakening, unrefreshing sleep, and daytime fatigue despite adequate time in bed. When these symptoms persist for months, they may indicate the kind of sleep dysfunction that eventually manifests as psychiatric disorders and cognitive decline.
The Technology Behind Recovery
Sleep Recovery’s use of brainwave entrainment technology represents a sophisticated approach to sleep restoration. Unlike sleeping pills, which suppress brain activity, the technology helps train the brain to produce healthy sleep patterns naturally.
The FDA-approved equipment works with the brain’s inherent self-intelligence to stabilize amplitude variables within the EEG flow globally. During sessions, clients’ brains gradually synchronize with these frequencies, learning to maintain the complex patterns needed for restorative sleep.
“We’re essentially teaching the brain to sleep properly again,” Wilson explains. “Once those patterns are reestablished, the brain can maintain them independently. That’s why the effects last long after the program ends.”
The BMJ study’s alarming findings about psychiatric disorders and dementia risk might seem discouraging, but Mayen’s sleep-focused perspective offers hope. If sleep dysfunction is indeed the common thread connecting mental health problems to cognitive decline, then effective sleep interventions could break this progression.
“The brain has remarkable capacity for recovery when you give it what it needs,” Mayen emphasizes. “Quality sleep is one of the most fundamental requirements for brain health. When we restore that, we often see improvements that surprise everyone – clients, families, and healthcare providers.”
This potential for recovery extends even to people who have struggled with multiple psychiatric conditions for years. Sleep Recovery regularly works with clients who have been diagnosed with depression, anxiety, and early cognitive problems. Many experience significant improvements across all these areas as their sleep quality is restored.
The key is recognizing that these seemingly separate problems may have a common origin in sleep dysfunction. This understanding opens new pathways for treatment and prevention that could help millions of people avoid the trajectory toward dementia.
Taking Action
For individuals experiencing poor sleep quality alongside mood or anxiety issues, the message is clear: don’t wait. The BMJ study shows that multiple psychiatric illnesses can increase dementia risk, but this progression isn’t inevitable if the underlying sleep dysfunction is addressed early enough.
By targeting the neurological foundations of healthy sleep, these approaches may prevent or reverse the trajectory toward dementia.
The program requires just 30-minute sessions every other day, making it accessible for people struggling with the energy limitations that often accompany sleep disorders and psychiatric conditions. Most importantly, the approach works with the brain’s natural healing capacity rather than suppressing symptoms with medications.
The connection between psychiatric disorders and dementia revealed in the BMJ study represents both a challenge and an opportunity. While the dramatically increased risk is concerning, understanding sleep as the potential common denominator offers a pathway for intervention.
For the millions of people struggling with multiple psychiatric conditions, this perspective offers genuine hope. Rather than accepting a trajectory toward cognitive decline, effective sleep intervention could restore brain health and prevent dementia.
To learn more about how sleep recovery can address the underlying dysfunction that connects psychiatric disorders to dementia risk, contact Sleep Recovery at (800) 927-2339 or visit https://sleeprecovery.net. The program that has helped thousands restore healthy sleep and reclaim their mental clarity may be the key to breaking the cycle revealed in this groundbreaking research.