Vagus Nerve Reset: How a Mysterious Organ Is Rewiring PTSD Recovery for Thousands
For years, people with treatment-resistant PTSD have faced a frustrating reality: traditional therapies work for about half of patients, and medications help roughly 40%, but a significant portion remains stuck with symptoms that disrupt every aspect of life. Now, groundbreaking research shows that stimulating a single nerve, the vagus nerve, might offer hope for those who haven’t found relief through conventional approaches.
The results from a small but promising study suggest that vagus nerve stimulation combined with therapy doesn’t just help people cope with trauma memories better. It appears to rewire the brain’s fear circuits at a fundamental level, addressing both PTSD symptoms and the sleep disruption that so often accompanies them.
What Makes PTSD So Stubborn
PTSD has been recognized in various forms since at least the Seven Years’ War in the 1750s when physicians documented excessive physical exhaustion, anger, irritability, and depression among soldiers. Whether called shell shock, battle fatigue, or its current name, the condition affects an estimated 6-7% of the civilian population and 13-14% of veterans.
What makes PTSD particularly challenging is how it rewires the brain’s threat detection systems. Unlike regular anxiety, PTSD stems from actual life-threatening experiences that leave lasting neurological imprints. The brain essentially gets stuck in survival mode, treating everyday situations as potential dangers and making it almost impossible to relax or feel safe.
Current treatments include cognitive processing therapy (helping people understand how they think about trauma), prolonged exposure therapy (gradually confronting traumatic memories in safe settings), and eye movement desensitization and reprocessing (EMDR). While these approaches help many people, they rely heavily on cognitive processing and conscious memory work.
The problem is that trauma often gets encoded in parts of the brain that operate below conscious awareness. Traditional talk therapies try to reach these areas through the thinking mind, but the neural pathways are sometimes too deeply entrenched to change through cognitive approaches alone.
Enter the Wandering Nerve
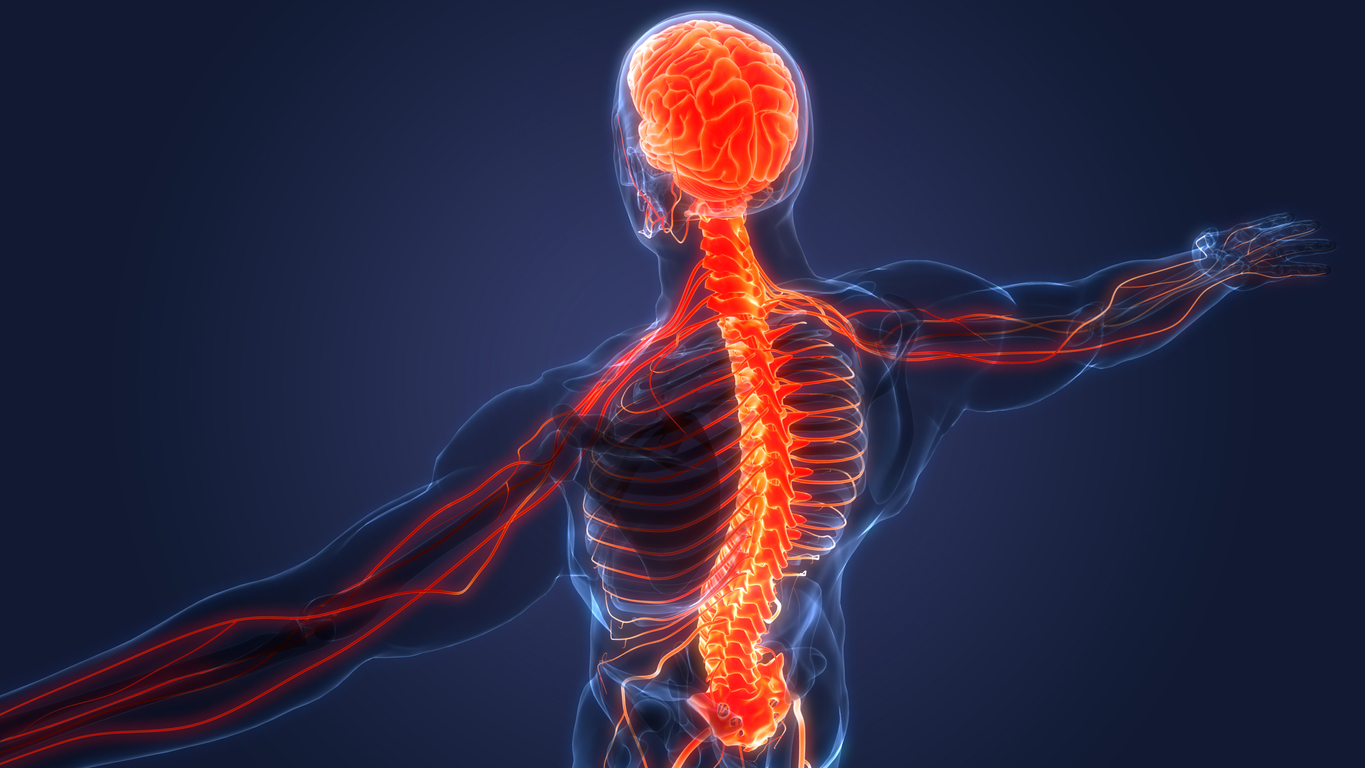
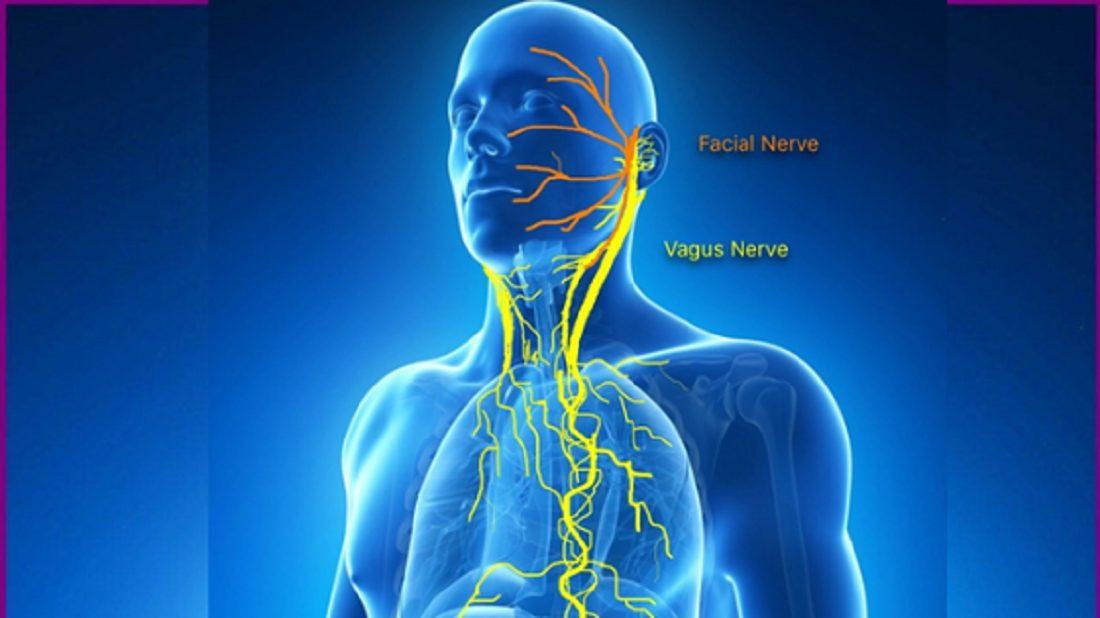
The vagus nerve derives its name from the Latin word for “wandering,” and it truly lives up to that description. Unlike other nerves that exit through the spinal cord, the vagus nerve travels directly from the brainstem throughout the body, connecting to most major organs and feeding sensory information back to multiple brain areas.
This extensive network makes the vagus nerve like the body’s internal internet, constantly communicating between the brain and organs about everything from heart rate and digestion to inflammation and sleep cycles. More importantly, for PTSD treatment, the vagus nerve connects directly to the brainstem, which serves as a relay station for higher brain functions.
Recent research has revealed that the vagus nerve is one of several critical “plasticity gatekeepers” systems that control the brain’s ability to change and adapt. When functioning correctly, these systems allow the brain to forge new neurological pathways and modify existing ones, which are essential for recovery from trauma.
The Breakthrough Study
The new research combined 12 sessions of prolonged exposure therapy with short bursts of vagus nerve stimulation, based on the idea that vagal stimulation enhances the brain’s ability to remodel traumatic memories. Nine participants had small devices implanted around their vagus nerve, which could deliver stimulation during therapy sessions and while doing therapeutic homework.
The results were remarkable. Of the seven participants who completed therapy, all achieved remission that lasted at least six months after treatment ended. This approach wasn’t just symptom improvement—these were people who met the full criteria for PTSD recovery across all measured domains.
What makes these results impressive is that all participants had treatment-resistant PTSD, meaning they hadn’t responded to previous therapy or medication attempts. The study showed no serious device-related side effects, suggesting that vagus nerve stimulation could be a safe option for people who’ve run out of alternatives.
The researchers concluded that vagal stimulation combined with therapy results in “adaptive changes in circuits associated with fear processing” and “indirectly enhances plasticity via widespread neuromodulatory release.” In simpler terms, the stimulation helped the brain fundamentally rewire its fear responses rather than just learning to cope with them better.
The Four-Chemical Orchestra
Understanding how vagus nerve stimulation works requires looking at four critical neurotransmitter systems choreographing brain maintenance and adaptation: norepinephrine, acetylcholine, GABA, and dopamine. Norepinephrine acts like a double espresso for the brain, powering up attention, arousal, and readiness to learn. It helps distinguish relevant stimuli from background noise, improving the signal-to-noise ratio in neural processing. Vagus nerve stimulation provides a norepinephrine-mediated increase in neural excitability, which improves memory and attention.
Acetylcholine enhances the encoding of new information and reinforces relevant patterns while pruning away neural noise. When we talk about neurons that “fire together, wire together,” we describe acetylcholine’s role in strengthening essential connections. Unfortunately, acetylcholine production declines with age, leading to memory problems and reduced learning capacity. Vagal stimulation works through the brainstem to enhance acetylcholine production.
Dopamine is the engine of motivation and reward, setting the tone for learning by reinforcing behaviors that lead to desired outcomes. Like norepinephrine, it helps the brain discern “what matters” by modulating signal-to-noise ratios in brain circuits. Vagus nerve stimulation indirectly enhances dopamine production through brainstem relay stations.
GABA acts as the brain’s primary brake system, creating the stability that learning requires. Rather than stifling brain plasticity, GABA defines boundaries and locks in stable circuits once learning has occurred. Vagal stimulation increases the brain’s inhibitory tone through brainstem connections, providing the balance needed for effective neural remodeling.
Beyond PTSD: Sleep and Recovery
One of the most significant but underappreciated benefits of vagus nerve stimulation may be its effects on sleep quality. The vagus nerve plays crucial roles in both inflammation regulation and sleep modulation, two factors that are severely disrupted in PTSD.
Through acetylcholine’s anti-inflammatory pathway, vagal signals suppress inflammatory chemicals called cytokines, reducing system-wide inflammation. It’s significant for people living with PTSD, who often show elevated inflammation markers that interfere with both mental health and sleep quality.
The vagus nerve also helps regulate the hypothalamic-pituitary-adrenal (HPA) axis, the body’s primary stress response system. PTSD typically involves chronic activation of this stress system, making it extremely difficult to achieve the deep relaxation necessary for restorative sleep.
Enhanced parasympathetic tone induced by vagal stimulation can improve sleep onset and deepen non-rapid eye movement (non-REM) sleep, facilitating restorative rest essential for trauma recovery. Many people with PTSD report that sleep problems are among their most debilitating symptoms, creating a vicious cycle where poor sleep worsens PTSD symptoms, which then further disrupts sleep.
What makes vagus nerve stimulation particularly exciting is how it leverages the brain’s natural capacity for neuroplasticity—the ability to modify, change, and adapt structure and function throughout life. We’ve moved far beyond the old belief that brains become fixed after childhood, understanding now that there are multiple critical periods when the brain remains highly adaptable.
Episodes that trigger PTSD may represent one of these critical periods when the brain becomes more plastic in response to extreme experiences. The problem is that this plasticity often gets channeled without proper support into forming stronger fear circuits rather than adaptive recovery patterns.
Vagus nerve stimulation redirects this plasticity toward healing by providing neuromodulatory support, allowing therapeutic interventions to create lasting changes. Instead of just teaching people to cope with traumatic memories, the combination helps the brain reprocess and integrate those memories in less distressing ways.
This redirect represents a fundamental shift from symptom management to actual healing. Rather than learning to live with PTSD, people may be able to resolve the underlying neural patterns that maintain the disorder.
The Technology Connection
Modern vagus nerve stimulation builds on decades of research but benefits from significant technological advances. Early devices were large and required major surgery, but current implantable stimulators are relatively small and can be precisely controlled.
Even more hopeful are medication-free approaches that stimulate the vagus nerve through the skin, offering similar benefits without requiring surgery. These transcutaneous devices could make vagus nerve stimulation available to more people, especially those not candidates for implanted devices.
This technological sophistication opens possibilities for combining vagus nerve stimulation with other advanced therapies. Concurrent vagal stimulation could enhance brain training technologies, neurofeedback systems, and even virtual reality therapy.
For people struggling with treatment-resistant PTSD, vagus nerve stimulation represents universal hope for breaking cycles that have persisted for years or even decades. The approach seems particularly promising for individuals whose symptoms include both emotional dysregulation and severe sleep disruption.
Healthcare providers are beginning to recognize that trauma recovery often requires addressing multiple systems simultaneously. Vagus nerve stimulation naturally targets several systems—fear processing, stress response, inflammation, and sleep—making it an efficient intervention for complex presentations.
The sleep benefits alone could be transformative for many people with PTSD. Quality sleep supports mental health recovery, from emotion regulation and memory consolidation to immune function and stress resilience. By addressing sleep problems at their neurological source, vagal stimulation may accelerate recovery across multiple domains.
Veterans organizations and trauma treatment centers are closely watching this research, recognizing that current approaches leave too many people without adequate relief. Combining vagus nerve stimulation with evidence-based therapy could become a new standard for treatment-resistant cases.
Looking Forward
While the initial research is up-and-coming, more robust research will be needed to confirm these findings and establish optimal treatment protocols. Researchers must determine which patients are most likely to benefit, what stimulation parameters work best, and how long treatment effects persist.
The implications extend beyond PTSD to other conditions involving dysregulated stress response systems and sleep disruption. Early research suggests vagus nerve stimulation might help with treatment-resistant depression, anxiety disorders, and even neurodegenerative conditions like dementia.
The approach is also consistent with the growing recognition that mental health conditions often involve whole-body systems rather than just brain chemistry. By targeting the vagus nerve’s multiple connections throughout the body, stimulation simultaneously addresses trauma’s effects on various physiological systems.
Perhaps most importantly, vagus nerve stimulation research advances our understanding of how the brain can heal from severe trauma. Rather than accepting that PTSD represents permanent damage, we’re learning that even deeply entrenched fear circuits can be modified through targeted interventions.
The Bottom Line
The sleep benefits make this research significant, given how central quality rest is to mental health recovery. For people whose trauma symptoms have been resistant to conventional treatments, vagus nerve stimulation may provide the neurological support needed to process and integrate traumatic experiences.
While more research is needed, the initial findings suggest that we’re moving toward a future where even the most severe trauma responses can be addressed through targeted, scientifically-based interventions. The brain’s capacity for healing is far greater than previously understood, and vagus nerve stimulation may be one key to unlocking that potential.
For the millions of people living with treatment-resistant PTSD, this research offers something that’s been in short supply: genuine hope for recovery. The wandering nerve that connects mind and body may also connect trauma sufferers to the possibility of reclaiming their lives from the grip of past experiences.
For more information on PTSD treatment, please call 800-927-2339 or visit: https://sleeprecovery,net