New Interventions for PTSD: Beyond Medication to Neurofeedback and Somatic Approaches

The Evolution of Trauma Treatment
Post-Traumatic Stress Disorder affects approximately 7-8% of Americans at some point in their lives. For decades, the primary treatment approaches involved a combination of psychotropic medications and talk therapy. While these methods help many individuals, a significant percentage continue to struggle with debilitating symptoms despite compliant treatment.
The limitations of traditional approaches have spurred research into alternatives that work with the brain and body in fundamentally different ways. Among the most promising developments are Alpha Theta Neurofeedback and Somatic Experiencing therapy, approaches that address trauma’s physiological imprints rather than focusing solely on cognitive or chemical interventions.
Medication-Based Treatment: The Current Standard
Conventional PTSD treatment typically relies heavily on medication. SSRIs (Selective Serotonin Reuptake Inhibitors) like sertraline and paroxetine remain the only FDA-approved medications specifically for PTSD. These are often combined with sleep aids, anti-anxiety drugs, and sometimes off-label use of antipsychotics for severe cases.
Dr. Bessel van der Kolk, psychiatrist and author of “The Body Keeps the Score,” notes that while medications can provide symptom relief, they rarely address the fundamental neurobiological patterns established by trauma. “Medications can take the edge off hyperarousal or help manage depression symptoms that accompany PTSD, but they don’t fundamentally rewire the trauma response patterns in the brain and nervous system.”
Many patients report significant downsides to medication approaches:
- Side effects range from weight gain and sexual dysfunction to emotional numbness
- Dependency concerns with benzodiazepines are often prescribed for anxiety symptoms
- Limited efficacy for core PTSD symptoms like flashbacks and emotional triggering
- The need for ongoing medication management, sometimes indefinitely
James R., a military veteran who spent three years on various medication combinations, shares: “The meds helped me function, but I felt like I was watching my life through a foggy window. I wasn’t getting triggered as easily, but I wasn’t living either.”
Alpha Theta Neurofeedback: Retraining the Traumatized Brain
Alpha Theta Neurofeedback represents a fundamentally different approach to trauma treatment. Rather than overriding brain chemistry with medications, it helps the brain recognize and modify its problematic patterns.
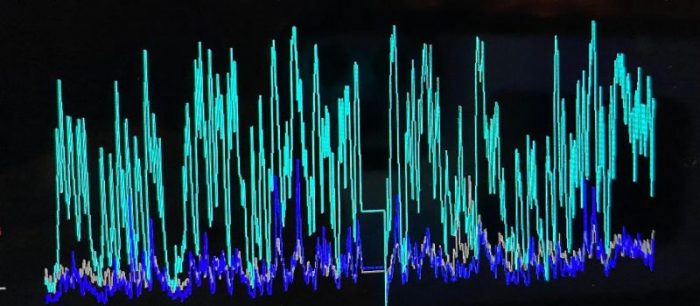
“Trauma creates distinctive patterns in brainwave activity,” explains Dr. Sebern Fisher, a pioneer in neurofeedback for trauma and author of “Neurofeedback in the Treatment of Developmental Trauma.” “People with PTSD typically show excessively high-frequency beta waves and abnormal patterns in the alpha and theta bands associated with relaxation and emotional processing.”
Alpha Theta Neurofeedback specifically targets these patterns. Sensors on the scalp monitor brainwave activity in real-time, while feedback (typically audio tones) signals when the brain produces more therapeutic patterns. The brain naturally gravitates toward patterns that generate positive feedback, gradually retraining.
David Mayen, Founder and Program Director at Sleep Recovery describes the process: “In Alpha Theta training, we guide the brain toward producing more alpha waves, associated with relaxed alertness, and theta waves, linked to emotional processing and trauma resolution. As the brain learns to move easily between these states, traumatic memories can be processed by the client without triggering the overwhelming fight-flight response that characterizes PTSD.”
The results can be profound. A landmark study by Peniston and Kulkosky found that Vietnam veterans with PTSD who received Alpha Theta training showed a 94% reduction in PTSD symptoms compared to control groups, with benefits maintained at a 30-month follow-up.
Critically, these improvements occur without the side effects associated with medications. The brain is not forced into new patterns through chemistry, but learning healthier functioning through natural feedback mechanisms.
Melissa T., a sexual assault survivor, found Alpha Theta Neurofeedback transformative after years of limited progress with medications and conventional therapy: “For the first time, I could think about what happened without feeling like I was right back in that moment. The constant vigilance, the panic attacks, the nightmares—they didn’t disappear overnight, but they steadily decreased with each session. After about 20 sessions, I felt like myself again, something I hadn’t experienced in years.”
EMDR vs. Somatic Experiencing: Body-Based Approaches to Trauma
Beyond brain-focused interventions, trauma treatment has increasingly recognized the body’s role in both maintaining and healing trauma. Two prominent approaches in this realm are Eye Movement Desensitization and Reprocessing (EMDR) and Somatic Experiencing.
EMDR, developed by Francine Shapiro in the 1980s, uses bilateral stimulation (typically eye movements) while a client recalls traumatic memories. This approach has substantial research support from organizations like the American Psychological Association.
However, EMDR comes with several potential drawbacks:
- The initial phases can temporarily increase distress as traumatic memories are activated
- The approach requires directly engaging with traumatic material, which some patients find overwhelming
- The structured protocol may feel rigid or mechanical to some clients
- A percentage of clients experience physical discomfort from the eye movements or other bilateral stimulation
Dr. Ruth Lanius, professor of psychiatry and director of the PTSD research unit at Western University, notes: “While EMDR is effective for many, some patients, particularly those with complex developmental trauma, find the direct memory engagement too activating, potentially reinforcing rather than resolving the trauma response.”
Somatic Experiencing, developed by Dr. Peter Levine, offers an alternative body-based approach that often addresses these limitations. Rather than directly processing traumatic memories, Somatic Experiencing focuses on resolving the physiological patterns established by trauma.
“Animals in the wild rarely develop trauma despite routine threats to their survival,” explains Dr. Levine in his book “Waking the Tiger.” “This is because they naturally complete the full defensive response cycle—moving from freeze or immobility back through fight-flight responses until reaching physiological completion. Humans often interrupt this cycle, leaving defensive energy trapped in the body.”
Somatic Experiencing guides clients in identifying and releasing these incomplete physiological responses. The approach is typically gentler than EMDR, working at the edge of comfort rather than diving directly into traumatic material.
Dr. Pat Ogden, founder of Sensorimotor Psychotherapy and expert in body-oriented approaches to trauma, explains: “Somatic approaches allow trauma processing to occur without requiring clients to re-experience traumatic events fully. By focusing on physical sensations and subtle movements, we help the body complete responses that were interrupted during traumatic experiences.”
Thomas R., who experienced childhood abuse, tried both approaches: “EMDR felt too intense for me. I would leave sessions completely wiped out, sometimes with migraines. With Somatic Experiencing, the process was slower but gentler. We worked with small sensations, and over time, I noticed I was less triggered in everyday situations without reliving the worst moments.”
The Sleep Connection: Addressing Insomnia and PTSD Together
Perhaps the most consistent symptom across PTSD cases is sleep disturbance. Between 70-91% of individuals with PTSD report significant sleep problems, with issues ranging from difficulty falling asleep to nightmares and middle-of-night panic.
“Sleep disruption isn’t just a symptom of PTSD—it’s a maintaining factor,” explains Dr. Jeffery Wilson, Clinical Director at Sleep Recovery. “Poor sleep reduces the brain’s ability to process emotional experiences and regulate stress responses, creating a vicious cycle where trauma symptoms lead to poor sleep, which then worsens trauma symptoms.”
Sleep Recovery’s program addresses this connection directly, recognizing that treating PTSD requires resolving sleep disruption concurrently.
“What makes our approach unique is that we don’t treat sleep and trauma as separate issues requiring separate interventions,” notes Mayen. “Our combined protocol uses specific Alpha Theta training parameters that simultaneously address trauma processing and sleep regulation.”
The protocol typically begins with stabilizing sleep patterns through targeted neurofeedback focused on normalizing the brain’s default mode network and reducing hyperarousal. As sleep improves, the protocol shifts toward deeper trauma processing using classic Alpha Theta training.
“The sequencing is critical,” continues Dr. Wilson. “When we restore healthy sleep first, clients gain the neurological resources needed for trauma processing. They become more resilient, making the trauma work more effective and less overwhelming.”
Catherine J., who developed PTSD following a serious car accident, found this approach transformative: “I tried sleep medications, but they left me groggy and didn’t stop the nightmares. Within two weeks of starting the Sleep Recovery program, I was sleeping through the night without medication. As my sleep improved, I found I could talk about the accident without feeling the same panic. The flashbacks gradually decreased, and three months later, I was driving again without anxiety.”
Integrating Approaches for Comprehensive Healing
While each approach shows promise individually, many trauma experts now recognize that integrated treatment protocols yield the best results, especially for complex or long-standing PTSD.
Sleep Recovery has embraced this integrated philosophy, offering protocols that combine:
- Alpha Theta Neurofeedback for Brain Pattern Normalization
- Somatic awareness techniques adapted from Somatic Experiencing
- Sleep-focused interventions to break the insomnia-PTSD cycle
- Practical tools for managing triggers in daily life
This comprehensive approach recognizes that sustainable recovery from trauma requires addressing both the neurological patterns established by traumatic experiences and their manifestations throughout the body and nervous system.
Frequently Asked Questions About New PTSD Interventions
Q: Do I need to taper off medications before trying neurofeedback or somatic approaches?
A: No. Alpha Theta Neurofeedback and Somatic Experiencing can both be used alongside medication. Many clients continue their prescribed medications initially, then work with their prescribing physician to reduce dosages as symptoms improve. Sleep Recovery coordinates with prescribing doctors to ensure safe and appropriate transitions.
Q: How many sessions are typically needed to see results?
A: Most clients report noticeable improvements in sleep within 4-6 sessions of neurofeedback. For full resolution of PTSD symptoms, the typical range is 20-40 sessions, depending on trauma complexity and duration. Somatic approaches often show gradual improvement throughout the process rather than dramatic shifts.
Q: Are the results permanent, or will I need ongoing treatment?
A: Unlike medication, which typically requires ongoing use to maintain benefits, neurofeedback appears to create lasting changes in brain function. Follow-up studies show that most clients maintain improvements years after completing treatment. Some clients benefit from occasional “booster” sessions during particularly stressful periods.
Q: How does neurofeedback compare to traditional exposure therapy for PTSD?
A: While exposure therapy requires clients to confront traumatic memories, potentially increasing distress temporarily directly, neurofeedback works with brain patterns without requiring conscious engagement with traumatic material. This process makes it particularly valuable for clients who find exposure approaches too overwhelming or have not responded.
Q: Will insurance cover these newer approaches to trauma treatment?
A: Coverage varies widely by provider. Some insurance plans cover neurofeedback for PTSD and other conditions, while others consider it experimental. Sleep Recovery works with clients to maximize insurance benefits when available and offers flexible payment options when insurance coverage is limited.

The Future of Trauma Treatment
As research continues to validate these newer approaches to trauma, they are increasingly moving from alternative to mainstream status. The Department of Defense has funded significant research into neurofeedback for PTSD in military populations, while the VA system has begun incorporating both neurofeedback and Somatic Experiencing at select facilities.
For individuals who have PTSD and related sleep disorders, this evolution represents genuine hope. Rather than managing symptoms indefinitely, these approaches offer the possibility of resolving trauma at its neurobiological source, restoring not just functioning but genuine well-being.
To learn more about Sleep Recovery’s integrated approach to PTSD and insomnia, visit https://sleeprecovery.net or call 1-800-927-2339 for a free consultation.
References:
-
State of the science: Eye movement desensitization and reprocessing (EMDR) therapy. https://onlinelibrary.wiley.com/doi/full/10.1002/jts.23012
-
Somatic experiencing – effectiveness and key factors of a body-oriented trauma therapy: a scoping literature review. https://pmc.ncbi.nlm.nih.gov/articles/PMC8276649/
- Somatic experiencing: using interoception and proprioception as core elements of trauma therapy. https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2015.00093/full
-
The effects of alpha/theta neurofeedback on personality and mood. https://pubmed.ncbi.nlm.nih.gov/15820636/
- An Alpha and Theta Intensive and Short Neurofeedback Protocol for Healthy Aging Working-Memory Training. https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2016.00157/full
-
Alpha-theta brainwave neuro-feedback therapy for Vietnam veterans with/ combative post-traumatic stress.https://fcpsych.com/alpha-theta-brainwave-neuro-feedback-therapy-for-vietnam-veterans-w-combative-post-traumatic-stress/ .
