Lack of Sleep Quality: Top Heart Disease Predictor for Women Over 45

New research reveals how poor sleep during menopause dramatically increases cardiovascular risks and what women can do about it.
The statistics are startling: cardiovascular disease remains the leading killer of women worldwide, yet only one in five women going through menopause achieves optimal heart health scores. Now, groundbreaking research from the University of Pittsburgh has identified an unexpected culprit behind this alarming trend. Among all the factors that influence heart health in midlife women, sleep quality has emerged as the most powerful predictor of future cardiovascular events and mortality.
This landmark study, published in the journal Menopause, analyzed health data from approximately 3,000 women who participated in the Study of Women’s Health Across the Nation (SWAN), an ongoing longitudinal study tracking midlife women across the United States. The researchers discovered that while four components of the American Heart Association’s Life’s Essential 8 assessment tool proved most critical for predicting future heart risks—blood glucose, blood pressure, sleep quality, and nicotine use—sleep quality stood out as the single most important factor for long-term cardiovascular health and survival.
The Sleep-Heart Connection: What the Numbers Tell Us
The research findings provide a clear picture of sleep’s significant impact on women’s cardiovascular health. Women who consistently achieved seven to nine hours of quality sleep each night demonstrated significantly better long-term heart health and increased longevity compared to their sleep-deprived counterparts. Conversely, those struggling with poor sleep patterns faced substantially elevated risks for heart disease and death from all causes.
Separate research tracking nearly 3,000 women over 22 years found that persistent insomnia symptoms increased heart disease risk by 70-75% compared to women with consistently good sleep patterns. The implications become even more sobering when considering that up to 50% of women experience sleep issues during midlife, a phase already marked by hormonal upheaval and increased stress.
Dr. Samar R. El Khoudary, the study’s senior author and professor of epidemiology at the University of Pittsburgh, emphasizes the significance of these findings. Previously, we’ve shown that the menopause transition is a time of accelerating cardiovascular risk. This study underscores that it’s also an opportunity for women to take the reins on their heart health.”
Why Women Over 45 Face a Perfect Storm
The menopause transition creates a perfect storm of cardiovascular vulnerability, making sleep quality particularly crucial. As menopause affects every middle-aged woman, many post-menopausal women suffer from increased risks for cardiovascular diseases and sleep problems simultaneously. The underlying mechanism involves the dramatic decline in estrogen levels that occurs during this life stage.
Estrogen is protective of the heart, and as it drops in the body, a woman’s risk of developing cardiovascular conditions, including heart disease, increases. This hormonal shift doesn’t just affect the cardiovascular system in isolation. Sleep disturbances are common during the transition, worsened by hormonal changes, vasomotor symptoms, and other factors that can increase with age and are linked to higher cardiovascular risk.
Menopausal women also tend to see a “sharp increased risk” for sleep apnea, which usually leads to worse sleep and a higher risk of heart issues. Sleep apnea, characterized by repeated breathing interruptions during sleep, creates additional strain on the cardiovascular system through oxygen deprivation and frequent sleep fragmentation.
Dr. Michael Grandner, director of the sleep health and research program at the University of Arizona, notes that women in this age group face a vulnerability to both heart health issues and sleep problems. Because women often juggle multiple challenges at this stage of life, such as being at the top of their careers and simultaneously caring for aging parents and teenagers, “they might just assume these sleep problems are due to stress.”
The Science Behind Sleep’s Cardiovascular Impact
Understanding how sleep deprivation damages the heart requires examining multiple interconnected biological pathways. The cardiovascular system relies on sleep for essential restorative processes that become disrupted when sleep quality deteriorates.
Blood Pressure Regulation. During normal, healthy sleep, blood pressure drops by around 10-20%, a phenomenon known as nocturnal dipping. Research highlights its crucial role in cardiovascular health, as non-dipping has been tied to an increased risk of stroke, heart attack, kidney problems, and reduced blood flow to the brain.
In hospitalized patients with sleep deprivation, there is a lack of the nocturnal dip in systolic and diastolic blood pressure, and a persistently activated sympathetic nervous system that results in elevated blood pressure. This disruption in the normal sleep-wake cycle can increase the risk of newly developed hypertension or worsening pre-existing elevated blood pressures.
Inflammatory Cascade. Experimental studies have shown that an acute decrease in the duration of sleep by a few hours over several days causes an increase in proinflammatory markers like C-reactive protein (CRP), which is believed to play a role in the pathogenesis of metabolic and cardiovascular diseases via inflammatory activation and vascular endothelial dysfunction.
Pro-inflammatory cytokines like IL-1, 6, and tumor necrosis factor (TNF) alpha are elevated in sleep-deprived individuals. This contributes significantly to the inflammatory component of vascular diseases, including strokes and coronary artery disease.
Autonomic Nervous System Disruption. Sleep deprivation is associated with elevated counterregulatory hormones among patients who have shortened or absent rapid eye movement (REM) sleep. This aspect of sleep regulates central nervous system activities during sleep. If it is reduced for any reason, it increases norepinephrine levels and predisposes to adverse cardiovascular events.
Metabolic Consequences: Lack of sleep may promote poor eating habits, which over time can contribute to poor nutrition, diabetes, and heart disease. Consistent lack of sleep is also linked to high blood pressure, increased risk of heart attack and stroke, poor blood sugar control, and obesity—all cardiovascular risk factors.
Sleep helps regulate the hormones that control hunger, and lack of sleep or sleep disturbances can trigger overeating and boost the desire for high-calorie foods. This creates a cascade effect where poor sleep leads to weight gain, which further compromises sleep quality and increases cardiovascular risk.
Beyond Duration: Quality Matters More Than Quantity
While most research focuses on sleep duration, emerging evidence suggests that sleep quality may be even more important for cardiovascular health. In the study, the sleep score was based on participants’ responses to three questions about their sleep habits over the past two weeks, focusing on trouble falling asleep, frequent night awakenings, and early morning awakenings with difficulty returning to sleep.
The research found that women who were peri- and postmenopausal who experienced a range of sleep disturbances scored worse on key measures of cardiovascular health than their premenopausal peers. This suggests that the fragmented, restless sleep common during menopause poses particular risks beyond simple sleep deprivation.
Dr. Brooke Aggarwal, an assistant professor of medical sciences in the cardiology division at Columbia University Medical Center, emphasizes that “women who are going through menopause should definitely keep an eye on their sleep habits and take this seriously. This is a critical period in a woman’s life, and there is much that can be done to reduce cardiovascular risks so women can live longer, healthier lives.”
The Sleep Recovery Program: A Comprehensive Approach to Better Sleep
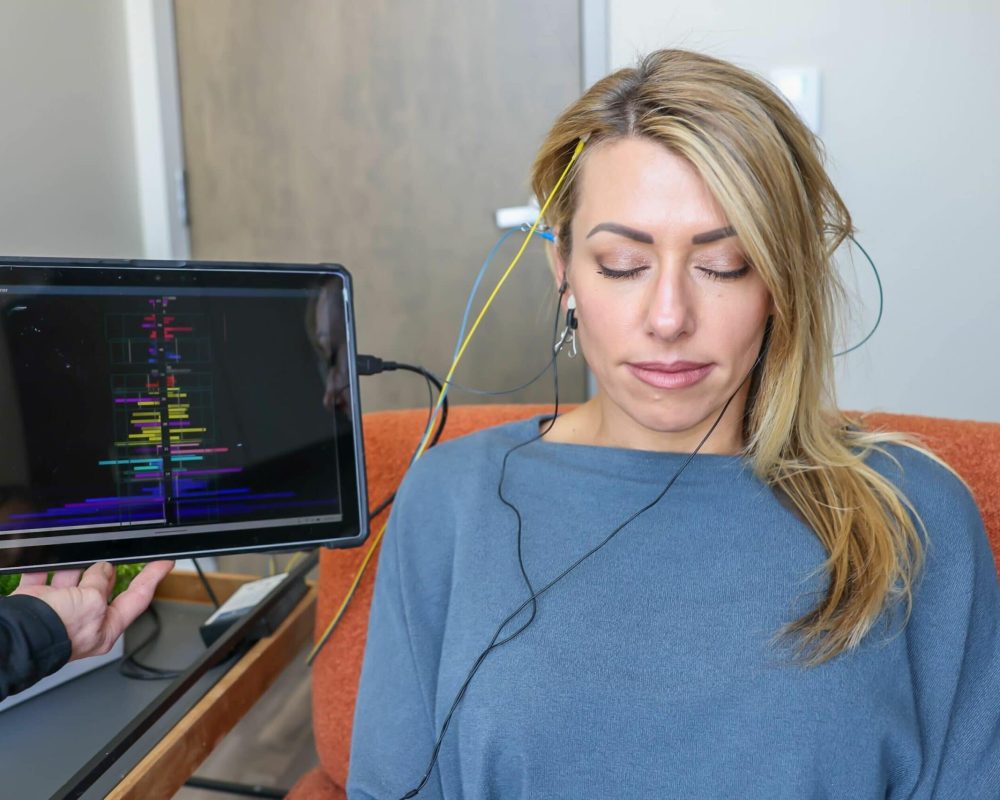
For women struggling with sleep issues that threaten their cardiovascular health, innovative solutions are emerging that address sleep problems at their neurological foundation. The Sleep Recovery Program utilizes safe, simple, and FDA-approved brainwave entrainment technology specifically designed for insomnia and anxiety.
Whether insomnia has been a problem for several weeks or years upon years, the Sleep Recovery Program has helped thousands of clients return to normal, healthy sleep that sustains itself for the long term. Just 30-minute sessions every other day are all it takes.
The program’s approach recognizes that sleep problems often stem from underlying brainwave instabilities that traditional sleep hygiene measures cannot address. Their software programs detect and correct brainwave instabilities at the source of most insomnia and anxiety issues. This process is safe, effective, and has no side effects whatsoever.
Program Goals and Outcomes The goal for new clients is 6.5 to 8.5 hours per night, 5 to 6 nights per week of restful sleep, and a mean average reduction of 85% in their overall anxiety. These targets align perfectly with the cardiovascular benefits identified in the recent research, potentially offering women a pathway to reduce their heart disease risk through improved sleep quality.
Specialized Support for Women The program recognizes that insomnia and anxiety are at epidemic levels for women all around the world. From career and family troubles to feeling a lack of security, women need a rapid and lasting solution for today’s problems. The approach includes personal coaching and phone support to prioritize clients’ needs, answer questions, and provide helpful dialogue throughout the recovery process.
Scientific Foundation: Brainwave entrainment is about recapturing performance. Just like cars, human brains run better with a full tune-up. The technology works by using specific audio frequencies to guide brainwaves into patterns associated with restful sleep, addressing the neurological disruptions that often underlie chronic insomnia.
The program’s effectiveness is supported by extensive client feedback, with verified Google reviews demonstrating the program’s success in helping individuals achieve sustainable sleep improvements. All phone consultations are provided free of charge and do not require signing up, making it accessible for women to explore whether this approach might benefit their specific situation.
Practical Steps for Protecting Heart Health Through Better Sleep
While innovative programs like Sleep Recovery offer advanced solutions, women can take immediate steps to improve their sleep quality and reduce cardiovascular risk:
Establish Consistent Sleep Scheduling: Try to go to bed and wake up at the same time every day. Consistency helps regulate the body’s internal clock and supports the natural blood pressure dipping that occurs during healthy sleep.
Create an Evening Routine. Have a routine that signals to your body that it’s time to sleep. It may include a relaxing shower or bath, turning off electronic devices, reading, or other relaxing activities.
Address Stimulant Consumption: Avoid stimulants such as caffeine near bedtime, as they may keep you awake. This is particularly important for women over 45, as caffeine sensitivity often increases with age.
Incorporate Regular Physical Activity. Try to get adequate exercise. Physical activity can help you get some ZZZs more quickly. However, timing matters—intense exercise too close to bedtime can be stimulating rather than sleep-promoting.
Seek Professional Evaluation. Women shouldn’t let anyone tell them that it’s just fatigue or that it’s just part of being in this age group. Professional sleep evaluation becomes crucial when self-help measures aren’t sufficient, particularly given the cardiovascular stakes involved.
Monitor for Sleep Disorders. Talk to your health care professional if you are approaching or in menopause and having trouble sleeping regularly. That’s because not all sleep problems have the same cause, and there could be another underlying cause, such as sleep apnea or a thyroid problem.
The Cardiovascular Medicine Perspective
Cardiologists are increasingly recognizing sleep as a critical component of heart health. Dr. Kathleen Drinan, a cardiologist at the University of Chicago Medicine, refers patients with atrial fibrillation and other arrhythmias for sleep evaluations. “Sleep disorders, especially untreated sleep apnea, can activate cardiac arrhythmias and elevate blood pressure, as well as lead to weight gain.”
The integration of sleep assessment into cardiovascular care represents a paradigm shift in how medical professionals approach heart disease prevention. Adults with 5 hours of sleep or less have a 200% to 300% higher risk of coronary artery build-up, meaning that sleep deprivation can increase coronary artery disease.
Looking Forward: Sleep as Preventive Medicine
The research linking sleep quality to cardiovascular outcomes in women over 45 represents more than an academic finding—it offers an actionable pathway for disease prevention. “This is such a positive place for menopausal women to focus, because it is a variable that can be measured and improved upon,” notes Dr. W. Christopher Winter, a neurologist and sleep medicine physician.
As Ziyuan Wang, the study’s first author and a Ph.D. candidate at Pitt Public Health, explains: “These findings suggest that healthy sleep in midlife could be a strong predictor of better heart health later in life.” However, Wang adds that future clinical trials are needed to confirm the impact of sleep on women’s heart health.
The implications extend beyond individual health outcomes to public health policy. With heart disease being the leading cause of death in women, these findings point to the need for lifestyle and medical interventions to improve heart health during and after menopause among midlife women.
The Bottom Line: Sleep Is Not a Luxury
For women over 45, quality sleep has emerged from the shadows as perhaps the most modifiable risk factor for cardiovascular disease. The research is clear: starting a good treatment plan could do more than make you feel well-rested the next day—it may support better heart health.
When it comes to women’s heart health, getting good sleep isn’t a luxury—it’s essential. The convergence of hormonal changes, increased life stressors, and physiological aging creates a critical window where sleep interventions can have outsized benefits for long-term cardiovascular health.
Whether through established sleep hygiene practices, professional medical intervention, or innovative approaches like the Sleep Recovery Program’s brainwave entrainment technology, women have more options than ever to address sleep issues before they translate into heart disease. The key is recognizing that sleep problems during menopause aren’t inevitable—they’re treatable conditions that deserve the same attention as blood pressure or cholesterol management.
As this research continues to evolve, one thing remains clear: the path to a healthy heart for women over 45 increasingly runs through the bedroom. Prioritizing sleep quality isn’t just about feeling rested tomorrow—it’s about protecting your heart for decades to come.
For more info on improving sleep quality, please call: 800-927-2339 or visit: https://sleeprecvoery.net


