Geriatric Insomnia
Coping With Sleep Challenges in Our Wisdom Years
Growing older doesn’t mean you have to give up on good sleep. Yet, for many seniors, the simple act of falling and staying asleep becomes increasingly elusive. Let’s explore this common but often misunderstood challenge facing our older population.
Understanding Age-Related Sleep Changes
Why Sleep Feels Different As We Age
Your sleep patterns naturally evolve:
- Lighter sleep becomes more common
- Sleep cycles shift earlier
- Wake times increase
- Sleep duration changes
- Recovery takes longer
But here’s what’s important to know – poor sleep isn’t just “part of aging.”
Common Challenges
Beyond Normal Age-Related Changes
Our older population often faces:
Physical Factors
- Chronic pain conditions
- Frequent bathroom visits
- Medication side effects
- Temperature regulation issues
- Joint discomfort
Environmental Impact
- Changed living situations
- Partner’s health issues
- Caregiving responsibilities
- Reduced physical activity
- Social isolation
The Medication Trap
Why Pills Aren’t Always the Answer
Many seniors turn to sleep medications, but consider this:
Risks for Older Adults
- Increased fall risk
- Morning grogginess
- Memory issues
- Balance problems
- Drug interactions
This makes finding natural solutions even more crucial for our elderly population.
Sleep Recovery’s Gentle Approach
Safe, Effective Solutions for Seniors
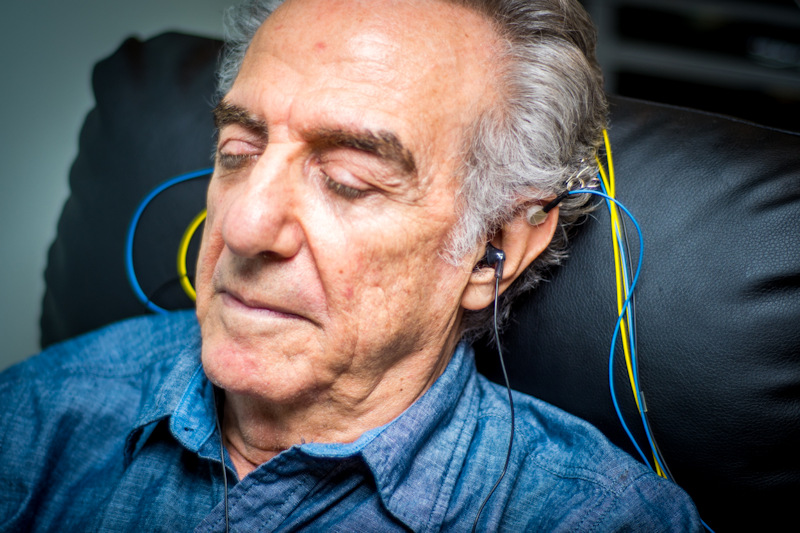
Sleep Recovery understands the unique needs of older adults:
Senior-Specific Benefits
- No medication risks
- Non-invasive brainwave training
- Comfortable, dignified treatment
- Respect for age-related concerns
- Support for caregivers
Their 15-session program addresses explicitly:
- Age-related sleep changes
- Chronic health conditions
- Medication interactions
- Mobility considerations
- Caregiver involvement
Most seniors see improvement within four sessions without the risks of traditional sleep medications.
Success Stories
Meet Dorothy, 78: “I thought poor sleep was just part of getting older. My doctor kept prescribing different pills, but they made me feel worse. Sleep Recovery’s approach restored my natural sleep – no medications needed.”
George, 82, shares: “After my wife passed, sleep became impossible. The relaxing neurofeedback helped me find peace again. Now I look forward to bedtime.”
Supporting Independence
Maintaining Dignity While Getting Help
Key considerations include:
Daily Routine Support
- Regular schedule maintenance
- Light exposure timing
- Activity level adjustment
- Social engagement
- Nutrition planning
Environmental Modifications
- Temperature control
- Noise reduction
- Lighting adjustments
- Comfort optimization
- Safety considerations
Role of Caregivers
Supporting Better Sleep
Caregivers can help by:
- Maintaining consistent routines
- Monitoring medication effects
- Encouraging appropriate activity
- Supporting treatment compliance
- Recognizing warning signs
Special Considerations
Understanding Unique Needs
Important factors include:
Health Conditions
- Chronic pain management
- Respiratory issues
- Heart conditions
- Neurological concerns
- Mobility limitations
Social Factors
- Living situation changes
- Loss of independence
- Partner health issues
- Family dynamics
- Social isolation
Creating Comfort
Making Sleep Inviting Again
Focus on:
Physical Comfort
- Appropriate bedding
- Temperature regulation
- Pain management
- Positioning support
- Environmental control
Emotional Security
- Familiar routines
- Comforting elements
- Social connection
- Anxiety reduction
- Sense of control
Frequently Asked Questions
Q: Is poor sleep inevitable with aging? A: While sleep patterns change, severe sleep problems aren’t typical for aging.
Q: How can neurofeedback help seniors specifically? A: It provides gentle, medication-free sleep improvement without side effects or fall risks.
Q: What role should family play in treatment? A: Family support enhances treatment success while maintaining senior independence.
Q: Are sleep medications safe for elderly adults? A: Many sleep medications pose significant risks for seniors, making natural alternatives preferable.
Q: How quickly can seniors expect improvement?A: Most see positive changes within 4-6 sessions of neurofeedback treatment.
Q: Can treatment accommodate mobility issues? A: Sleep Recovery’s program adapts to individual needs and limitations.
Professional Support
Working with Healthcare Teams
Coordination includes:
- Primary care physicians
- Specialists
- Physical therapists
- Mental health professionals
- Social workers
Conclusion
Aging doesn’t mean giving up on good sleep. With proper support, understanding, and treatment approaches like Sleep Recovery’s neurofeedback program, seniors can regain restful sleep without relying on risky medications.
The golden years should be comfortable and restful. Let’s work together to make that possible through safe, effective sleep solutions that respect our older population’s dignity and unique needs.
References
- NIH: Insomnia in Older Adults. https://pmc.ncbi.nlm.nih.gov/articles/PMC7731454/#:~:text=Recent%20Findings,%2C%20cognitive%20function%2C%20and%20dementia.
- Insomnia in the Elderly: Cause, Approach, and Treatment. https://www.amjmed.com/article/S0002-93430501056-9/fulltext
-
The effects of insomnia on older adults’ quality of life and daily functioning: A mixed-methods study. https://www.sciencedirect.com/science/article/abs/pii/S019745722030149X
- Neurofeedback and the Aging Brain: A Systematic Review of Training Protocols for Dementia and Mild Cognitive Impairment. https://pmc.ncbi.nlm.nih.gov/articles/PMC8221422/
-
Effectiveness of Electroencephalography Neurofeedback for Improving Working Memory and Episodic Memory in the Elderly: A Meta-Analysis. https://www.mdpi.com/1648-9144/60/3/369
Age brings wisdom, and with the proper support, it can also bring peaceful sleep. Let’s help our seniors find the rest they deserve.
