CBTi Pros And Cons: Why Your Heart May Still Be at Risk

A new study presented at the 2024 SLEEP Conference revealed something most Americans don’t know: 123 million adults across the Americas are living with chronic insomnia disorder. That’s 37 million people in the United States alone—roughly one in six adults trapped in a cycle of broken sleep that researchers now recognize demands urgent policy intervention.
The lead investigator’s statement was direct: these findings underscore an urgent need for enhanced clinical care pathways because insomnia doesn’t just affect sleep quality and daily functioning. It has broader implications for entire public health systems. What he didn’t say—what most patients never hear—is that the current treatments being recommended aren’t addressing the most dangerous part of this crisis.
Your doctor finally takes your insomnia seriously. After months of broken sleep and exhausted days, you’re referred to a cognitive behavioral therapist who promises lasting results. Eight weeks later, you’re sleeping better—six hours instead of four, falling asleep faster, waking less often. Success, right?
Not quite. While you’re celebrating better sleep, something more concerning may be happening inside your body. Your heart is still under attack. Your blood vessels are still inflamed. Your cardiovascular system is still aging faster than it should. The treatment that fixed your sleep symptoms left the most dangerous consequences completely untouched.
Hidden Truth Most Experts Don’t Mention
Here’s what almost no one is telling insomnia patients: the standard treatments being prescribed right now, even gold-standard ones, are not protecting your heart. Recent research published in Circulation Research makes this point impossible to ignore. While cognitive behavioral therapy for insomnia has become the recommended first-line treatment, clinical trials still haven’t demonstrated whether it actually reduces the cardiovascular risks that make chronic insomnia so deadly.
And according to the 2024 analysis, even this imperfect treatment isn’t reaching most people who need it. The shortage of trained CBT-I practitioners means millions of Americans with chronic insomnia aren’t getting any treatment at all, let alone one that might address the cardiovascular damage accumulating in their bodies.
Think about that for a moment. We know insomnia damages your heart. Studies show that chronic insomnia increases your risk of coronary heart disease by 45%, raises your chances of developing hypertension, diabetes, heart failure, and stroke. Yet the treatment everyone is being sent to hasn’t been proven to prevent any of that damage, and most people can’t even access it in the first place.
The Cardiovascular Time Bomb
That 123 million figure from the 2024 study isn’t static. Evidence suggests that the prevalence of insomnia is growing over time, which means the cardiovascular burden is expanding alongside it. Women are hit particularly hard, representing nearly 60% of all insomnia cases across the Americas.
The connection between insomnia and heart disease goes far beyond feeling tired. When you can’t sleep night after night, your body enters a state of chronic physiological stress that tears apart your cardiovascular system at the molecular level.
Your sympathetic nervous system stays locked in fight-or-flight mode, flooding your bloodstream with stress hormones around the clock. Your heart rate variability—one of the best predictors of cardiovascular health—becomes erratic and blunted. Blood pressure that should drop during sleep stays high, eliminating the natural recovery period your heart desperately needs.
Full Body Inflammation Factors
The inflammatory damage is equally brutal. Chronic insomnia drives up C-reactive protein, interleukin-6, and tumor necrosis factor-alpha; the same inflammatory markers linked to atherosclerosis and heart attacks. Your hypothalamic-pituitary-adrenal axis becomes dysregulated, pumping out excess cortisol that accelerates arterial stiffness and vascular damage.
A 2017 meta-analysis examining over a million patients found that people with insomnia symptoms face a 13% higher risk of cardiovascular disease overall. Research from the Multi-Ethnic Study of Atherosclerosis demonstrated that people sleeping under seven hours with insomnia symptoms had dramatically greater cardiovascular reactivity to stress compared to normal sleepers.
One large-scale study found that optimal sleep patterns at age 30 translated into 4.7 additional years of life expectancy for men and 2.4 years for women compared with those with standardsuboptimal sleep quality. Chronic insomnia accelerates epigenetic aging, meaning your cells literally age faster than they should.
Yet despite all this evidence about cardiovascular damage, the treatments being handed out don’t address it.
The CBT-I Blind Spot
The 2024 research revealed another troubling reality: cognitive behavioral therapy for insomnia—the treatment everyone agrees should be first-line—isn’t widely accessible. There’s a shortage of trained CBT-I practitioners. Most people with insomnia never even get diagnosed, let alone treated with the recommended approach.
But even for those who do access CBT-I, there’s a problem nobody is talking about.
Cognitive-behavioral therapy for insomnia has an impressive track record of improving sleep. Meta-analyses show it reduces insomnia symptoms by roughly 50% after treatment, with effects lasting up to two years. Patients sleep longer, fall asleep faster, and wake less often. These are genuine improvements that matter to people’s daily lives.
But improving sleep symptoms isn’t the same as reversing cardiovascular damage.
A Second Study
A 2025 systematic review in the Journal of Clinical Sleep Medicine examined whether CBT-I actually improves cardiovascular outcomes in patients with existing heart disease. The results were telling. While CBT-I helped address the behavioral aspects of insomnia, the review acknowledged that “limited sample size encourages more robust evidence from high-quality, large-scale trials with long-term follow-up” regarding cardiovascular effects.
Another recent analysis put it even more directly: clinical trials testing CBT-I in cardiovascular patients are still trying to determine whether the treatment impacts cardiovascular risk factors at all. They’re measuring blood pressure dipping, vascular function, sympathetic nervous system activity, and atherosclerotic risk scores to see if improvements in sleep translate to improvements in heart health. The fact that researchers are still asking this question, after years of CBT-I as the standard treatment, tells you everything about what hasn’t yet been proven.
The problem isn’t that CBT-I doesn’t work for sleep. The problem is that fixing sleep behavior doesn’t automatically fix the neurological dysregulation driving both the insomnia and the cardiovascular damage.
Why Medications Miss the Mark Too
Prescription sleep medications create their own set of problems. While they can knock you out, they don’t produce natural sleep architecture. The sedation isn’t the same as restorative sleep, and many medications actually suppress the deep sleep stages where cardiovascular recovery happens.
Studies consistently show that sleep medications lose effectiveness over time, requiring higher doses for the same effect. Long-term use has been linked to increased mortality risk in multiple large-scale studies. And when patients try to stop, they face rebound insomnia that’s often worse than what they started with.
Just as troubling, medications do nothing to address the neurological patterns driving the problem. The hyperarousal remains. The stress response stays activated. The cardiovascular damage continues to accumulate under the chemical suppression.
A Different Approach: Training the Brain Directly
At Sleep Recovery, Inc., we take a fundamentally different approach. Rather than teaching sleep strategies or prescribing medications, we use neurofeedback and brainwave entrainment to directly address the neurological dysregulation driving both insomnia and its cardiovascular consequences.
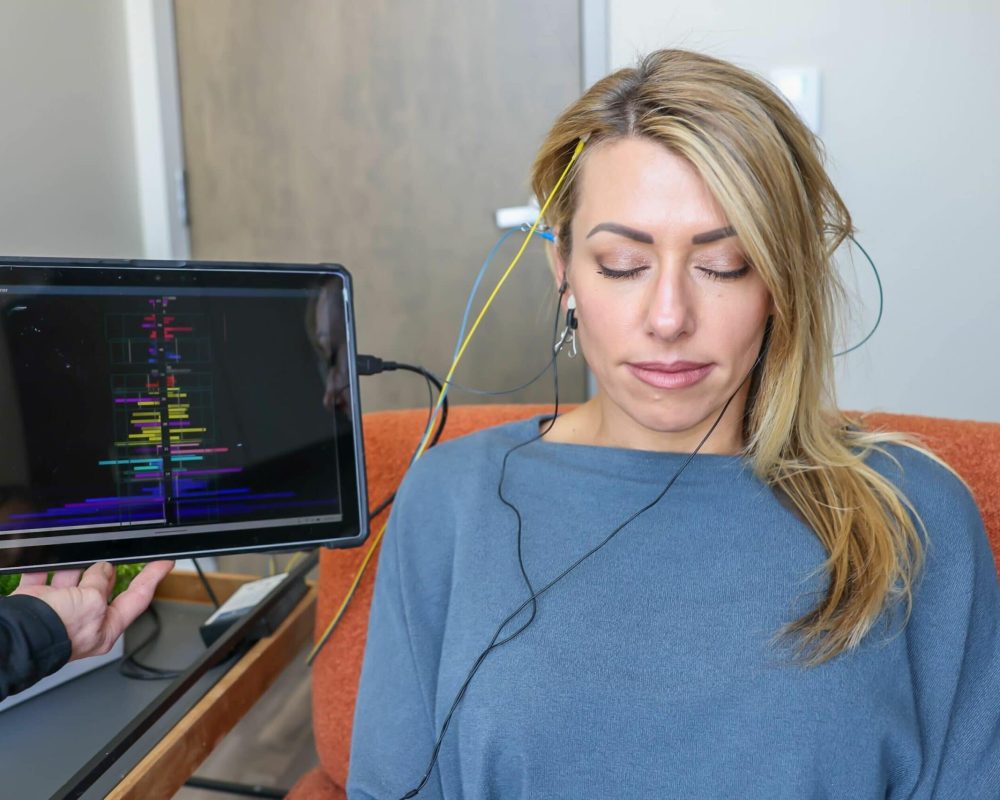
We start with a quantitative EEG assessment that maps your brain’s electrical activity with precision. This shows us exactly where your brain is stuck in patterns of hyperarousal, stress reactivity, and autonomic dysfunction. We’re not guessing about what might be wrong—we’re seeing it in real-time brain activity.
What’s Involved in Sessions?
Then we use that information to create a personalized training protocol. During neurofeedback sessions, you sit comfortably while sensors monitor your brainwave activity. The moment your brain produces healthier patterns—reduced hyperarousal, better alpha wave production, more balanced autonomic function—you receive immediate feedback through changes in audio or visual displays.
Your brain learns through this reinforcement. Session by session, it discovers how to shift out of the dysregulated patterns that have been driving your insomnia and cardiovascular stress. We’re not forcing anything or suppressing anything. We’re teaching your brain a skill it has forgotten or never properly developed.
The sessions themselves are straightforward—30 minutes every other day. No homework. No sleep restriction protocols that leave you more exhausted in the short term. No medications to take or side effects to manage.
Research on alpha neurofeedback training shows measurable improvements in both anxiety and sleep quality that last for months after training ends. Studies examining neurofeedback for generalized anxiety disorder found significant reductions in anxiety traits and depressive symptoms, with corresponding improvements in insomnia severity.
What makes this relevant to cardiovascular concerns is that we’re addressing the root causation: the neurological EEG dysregulation that produces both sleep disruption and the chronic stress response that damages your heart. When the brain learns to regulate its arousal states more effectively, when your autonomic nervous system achieves better balance, when your stress reactivity normalizes—the downstream effects touch everything. Sleep improves. Anxiety decreases. And the relentless cardiovascular assault begins to ease.
Our typical client sees their sleep improve to 6.5-8.5 hours per night. Anxiety levels drop by roughly 85% as measured by standardized assessments. But just as significantly, they report feeling calmer during the day, handling stress more easily, experiencing fewer panic symptoms, and noticing their racing thoughts quiet down. These aren’t just symptom improvements—they’re signs of fundamental neurological change.
Beyond Sleep: Addressing the Whole Problem
The cardiovascular consequences of chronic insomnia exist because insomnia isn’t just a sleep problem—it’s a nervous system problem. The same dysregulation that keeps you awake at night is the dysregulation that’s damaging your heart during the day.
This is what the researchers presenting at the 2024 SLEEP conference meant when they called for comprehensive care strategies. They recognized that standard treatment focusing narrowly on sleep symptoms misses the broader health implications. Teaching better sleep habits might help you fall asleep faster, but it doesn’t calm the chronic stress response that’s elevating your inflammatory markers. Medications might sedate you into unconsciousness, but they don’t restore the natural autonomic balance your cardiovascular system needs to recover.
Holonomic-Based EEG Amplitude Training
Specific neurofeedback training addresses the actual problem: a nervous system stuck in patterns of chronic arousal and stress reactivity. When that changes—when your brain learns to regulate itself more effectively, both the insomnia and the cardiovascular stress improve together.
This is why we frame what we do as brain efficiency training rather than sleep treatment. Sleep is one of many things that improve when your brain is functioning better. Your heart health is another. So is your emotional regulation, your resilience to stress, and your overall quality of life.
After 17 years and over 4,000 clients, we’ve seen this pattern repeat itself consistently. When the underlying neurological dysfunction is addressed directly, the ripple effects extend far beyond just sleeping better at night.
What This Means for You
The researchers who presented at the 2024 SLEEP conference were clear: we need comprehensive care strategies and enhanced clinical pathways to address this crisis. They recognized that current approaches aren’t meeting the scale or severity of the problem.
What they’re calling for is exactly what brain training through neurofeedback provides: a comprehensive solution that addresses the neurological dysfunction underlying both sleep disruption and cardiovascular damage.
If you’re one of the 37 million Americans living with chronic insomnia, especially if you’ve tried standard treatments without getting the lasting relief you need, you deserve to know the whole story. The recommended first-line treatment isn’t widely accessible—and when you can access it, it hasn’t been shown to protect your cardiovascular health.
You have the right to consider an approach that addresses the root cause rather than managing symptoms. Brain training through neurofeedback offers something fundamentally different: the possibility of actually fixing what’s broken rather than just coping with it.
Your brain created these dysfunctional patterns. With the proper training, it can unlearn them. Your nervous system got stuck in a state of chronic stress reactivity. With targeted intervention, it can return to healthy regulation.
We’ve been doing this work in Irvine for 17 years because we’ve seen it change lives, not by teaching sleep strategies or prescribing pills, but by giving people’s brains what they actually need: practical, direct training that restores healthy function.
If you’re ready to address both your sleep and the hidden cardiovascular damage left by standard treatments, we’re here to help. Contact Sleep Recovery Center to schedule a consultation and learn whether neurofeedback training is proper for you.
Your heart deserves the same attention as your sleep symptoms are getting. It’s time both got the solution they need.
