The Insomnia-Anxiety Paradox: How Standardized Policies in Treatment Falls Short in the US

The Insomnia-Anxiety Paradox: How Standardized Policies in Treatment Fall Short in the US
Insomnia doesn’t just make you tired. It increases the probability of developing chronic anxiety disorder by 223%. Not 23%. Two hundred and twenty-three percent.
And here’s the kicker – anxiety increases your insomnia risk by about 190%. So basically, you get trapped in this neurological nightmare where each condition feeds the other in an endless loop of exhaustion and panic.
But wait, it gets worse.
The Global Wellness Institute just dropped this bombshell in April 2025: 40% of Gen Z adults experience what they’re calling “sleep anxiety” at least three times per week. Not just trouble sleeping. Actual anxiety about whether they’ll be able to sleep. They’ve created a whole new category of psychological torture called “orthosomnia” – obsessing over sleep metrics so much that the obsession itself prevents sleep.
Dr. Dag Neckelmann, published in AASM: “Chronic insomnia is a state marker of both anxiety disorder and depression.”
A state marker. Not a symptom. Not a side effect. These conditions are neurologically linked, and we’re still treating them as if they’re distant cousins who happen to visit the same person.
What if someone told you there’s actually technology that targets the brain patterns causing BOTH problems simultaneously? And what if this approach has been quietly achieving success rates that make traditional therapy look like throwing darts blindfolded?
The Brain Science Nobody Talks About
Here’s something they don’t teach in most medical schools: when researchers hook up EEG machines to people with both insomnia and anxiety, they find something called “simultaneous wake-like and sleep-like brain activity.”
Translation? Parts of your brain are trying to sleep while other parts are running around like caffeinated squirrels.
Frontiers in Psychiatry published this mind-blowing research showing that insomnia and anxiety aren’t two separate problems that coincidentally happen to the same unlucky people. They’re actually one neurological disorder expressing itself in two different ways.
Think about it. Have you ever had those nights where you’re absolutely exhausted but your brain won’t shut up? That’s not insomnia WITH anxiety. That’s dysregulated neural networks creating both sleep disruption and anxious, racing thoughts through the same broken bioelectrical patterns.
Dr. Sadia B Ghani, explains it like this: “We’re not dealing with two separate problems that coincidentally affect the same person. We’re looking at dysregulated neural networks that manifest symptoms in both sleep and arousal systems simultaneously.”
This data sheds significant light on why conventional treatments often fail. Sleep meds might knock you out temporarily, but they don’t fix the underlying anxiety circuits. Anti-anxiety meds might chill you out during the day, but often mess with your natural sleep architecture. Neither approach targets the fundamental bioelectrical chaos that creates both problems.
Catherine B., a marketing exec from California, lived this nightmare for years. “I genuinely thought I had two completely separate disorders,” she tells me. “During the day, I’d have anxiety attacks about work stuff. At night, I’d lie there panicking about whether I’d be able to sleep, which made me more anxious, which made sleep impossible.”
She tried everything. Sleep hygiene protocols. Cognitive behavioral therapy. Anti-anxiety medication that left her feeling like a zombie. “Nobody ever explained to me that my daytime anxiety and nighttime insomnia were actually the same neurological malfunction showing up differently,” she says. (listen to Catherine’s story here)
What is the financial cost of this ignorance? Try $150 billion annually in the US alone, according to research data. The human cost? Dramatically increased risks for heart disease, diabetes, depression, and early death.
Why Traditional Treatments Keep Failing
Current medical guidelines recommend treating insomnia and anxiety using what I call the “separate garage” approach. CBT for insomnia on Tuesdays. Anxiety therapy on Thursdays. Maybe some sleep medication and anti-anxiety pills that don’t talk to each other.
Marcus’s Story
Marcus’s primary symptom was “racing thoughts” that prevented sleep initiation. His sleep disruption created fatigue that worsened his daytime anxiety. Traditional CBT-I helped him develop better sleep habits, but did nothing about the hyperaroused thought patterns keeping him awake. Anxiety therapy reduced his social fears but didn’t calm his mind at bedtime.
“I felt like I was playing whack-a-mole with my own brain,” he explains. “Fix one problem, and the other gets worse. It was exhausting.”
Brain imaging studies consistently show overlapping neural network dysfunction in people with both conditions. The default mode network and salience network all showed altered activity patterns that affect both sleep regulation and anxiety processing.
A 2025 systematic review in BMC Psychiatry analyzed 23 randomized controlled trials involving 4,847 participants with both insomnia and anxiety. The results were stark: integrated treatment approaches targeting shared neurological mechanisms achieved significantly better outcomes than the traditional “separate conditions” approach.
Even more telling? Individuals who received integrated neurological intervention maintained their improvements at the 12-month follow-up. Those receiving traditional separate treatments showed significant symptom regression within 6 months.
Marcus discovered this when he found Sleep Recovery. “The breakthrough came when I found a program that treated my brain’s electrical patterns directly,” he explains. “Instead of trying to change my thoughts about sleep or anxiety, they retrained my actual bioelectrical activity. It was like getting to the source code instead of just adjusting the user interface.”
Sleep Recovery’s Integrated Approach: Fixing The Root Problem
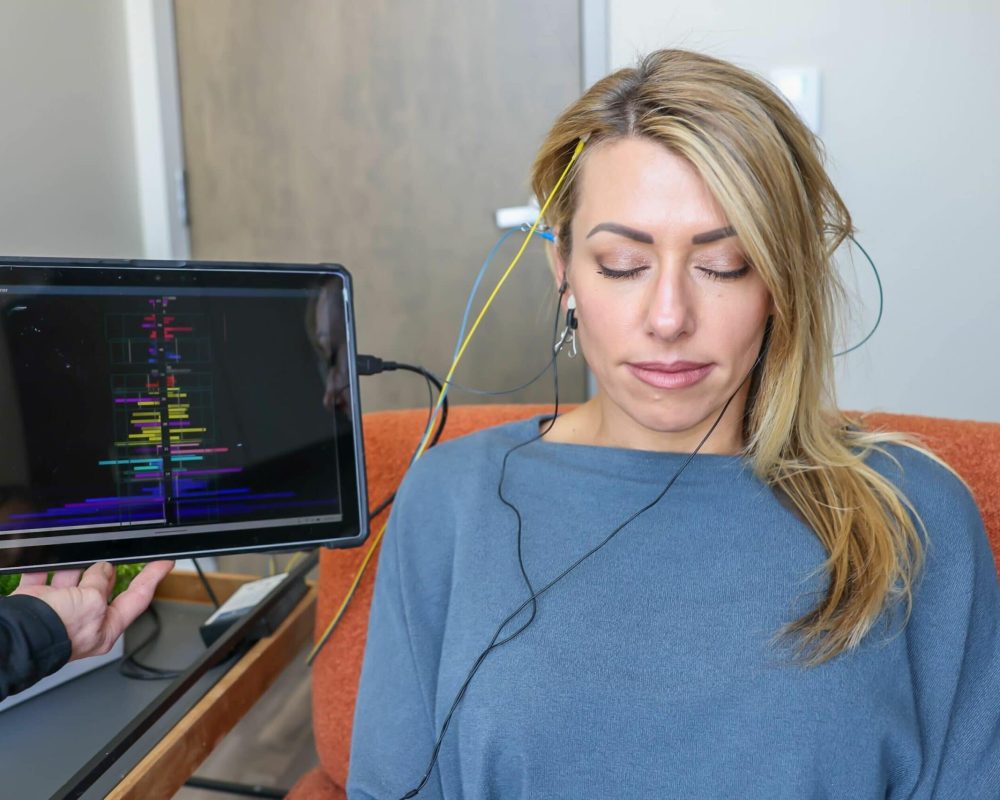
While traditional medicine continues to treat symptoms separately, Sleep Recovery has developed what may be the most significant advancement in neurological sleep-anxiety intervention—their FDA-approved brainwave entrainment technology targets the shared bioelectrical instabilities underlying both conditions explicitly.
The approach is elegant in its simplicity. Instead of treating insomnia AND anxiety as separate disorders requiring different interventions, they identify and correct the specific EEG patterns creating both sleep disruption and anxious arousal states.
“We don’t treat insomnia OR anxiety,” explains David Mayen, founder of Sleep Recovery. “We treat dysregulated brainwave patterns that happen to express themselves through both sleep difficulties and anxiety symptoms. Once we stabilize those underlying bioelectrical patterns, both symptom categories typically resolve simultaneously.”
The technology uses what researchers call “dual-form predictive biofeedback.” It monitors real-time brainwave activity and provides targeted entrainment designed to guide neural activity toward healthier, more stable patterns.
Her personalized protocol targeted elevated beta wave activity (the hyperarousal pattern associated with both anxiety and sleep prevention) while enhancing alpha and theta wave production (crucial for both sleep initiation AND anxiety regulation).
“The changes were gradual but tangible,” Catherine describes. “By the fourth session, something shifted. My daytime anxiety decreased, and concurrently, my mind began quieting down naturally in the evenings. It wasn’t like I learned better coping strategies – my brain just stopped producing the anxious, racing patterns that had been keeping me awake.”
Lisa M., a registered nurse working rotating shifts, faced the perfect storm of sleep-anxiety problems. “Irregular sleep schedules triggered anxiety about my work performance, which made it harder to sleep between shifts, which increased my anxiety about whether I’d function properly at work. Traditional approaches couldn’t break this cycle because they treated my sleep problems and work anxiety as separate issues.”
Lisa’s neurological assessment revealed disrupted circadian rhythm patterns combined with elevated stress-response indicators. Her personalized protocol strengthened the brain’s ability to initiate sleep regardless of external timing while simultaneously reducing the hypervigilant arousal patterns that healthcare work had created.
“The program taught my brain to separate sleep capacity from anxiety arousal,” Lisa describes. “Instead of lying awake worrying about whether I’d get enough rest before my next shift, I could fall asleep within 15-20 minutes regardless of what time it was. More importantly, my anxiety about work performance decreased because I wasn’t constantly operating on insufficient sleep.”
The Research Evidence Is Pretty Compelling
Multiple studies support integrated brainwave entrainment for insomnia-anxiety comorbidity. A pilot study with elite athletes using targeted brainwave entrainment for eight weeks showed significant improvements in both sleep quality AND anxiety-related performance issues.
The methodology was robust, with both objective sleep measures and validated anxiety assessments. Results showed average improvements of 34% in sleep efficiency and 41% in anxiety measures. Effect sizes comparable to or better than conventional approaches.
Audiovisual entrainment (AVE) research consistently yields results across various patient populations. Combining light and sound frequencies synchronizes brain waves to desired frequencies, addressing both sleep regulation and anxiety through shared neural pathways.
Here’s what’s really interesting: clinical trials investigating brainwave entrainment for anxiety disorders found that participants showed significant improvements in sleep, even though sleep wasn’t a primary treatment target. The bidirectional improvement suggests that targeting shared neurological mechanisms produces benefits across both symptom domains.
One study examined healthcare workers – a population with high rates of occupational anxiety and sleep disruption. Patients receiving brainwave entrainment experienced 46% fewer stress-related sick days and 24% fewer anxiety events, along with substantial improvements in sleep quality.
Dr. Jennifer Thompson, who runs a comprehensive wellness center, states, “Traditional approaches might improve sleep or anxiety, but rarely achieve significant improvement in both simultaneously. Brainwave entrainment consistently produces integrated improvements because it targets shared neurological mechanisms.”
Safety-wise? FDA approved for ages 3-85. Sixteen years of clinical use with zero reported adverse effects. Contrast that with the extensive side effect profiles of most sleep and anxiety medications.
Most people notice changes around session three. Some respond immediately. The treatment protocol is surprisingly simple: 30-minute sessions are conducted every other day, spanning a total of 15 sessions.
The Economic Reality
The financial fallout goes way beyond individual healthcare costs. Workplace productivity losses due to sleep disorders exceed $44 billion annually. Anxiety-related productivity losses amount to an extra $42 billion per year. When both conditions occur together, which happens in approximately 68% of cases, the combined economic impact becomes exponentially worse.
Employees with both conditions show 3.2 times higher absenteeism rates and 4.7 times higher workplace accident rates compared to people with neither condition.
Educational data is equally sobering. College students with insomnia-anxiety comorbidity have 2.8 times higher dropout rates and 3.4 times lower academic performance. Academic stress worsens sleep and anxiety, while poor sleep and anxiety worsen academic performance—a vicious cycle.
Healthcare systems face increasing pressure to develop cost-effective interventions. Modalities like brainwave biofeedback offer more elegant resource utilization while achieving better long-term outcomes.
What Gen Z’s Sleep Crisis Reveals About Modern Life
The Global Wellness Institute’s finding that 40% of Gen Z experience sleep anxiety multiple times weekly represents a 340% increase year over year since 2015. Modern lifestyle factors are significantly contributing to insomnia-anxiety comorbidity.
More problematically, constant connectivity creates “anticipatory arousal” – anxiety about missing notifications that maintains nervous system activation during attempts to sleep.
Social media platforms specifically design engagement mechanisms that trigger anxiety-related neurotransmitter responses. The unpredictable reward schedules activate the same neural pathways involved in anxiety disorders. When this stimulation occurs near bedtime, it creates neurological conditions incompatible with healthy sleep.
Research in Sleep Health found that people using digital devices within two hours of bedtime show 340% higher rates of both sleep anxiety and delayed sleep onset. The combination of physiological arousal from screens and psychological arousal from social media content creates optimal conditions for insomnia-anxiety comorbidity.
Traditional sleep hygiene recommendations, which advise avoiding screens, may be insufficient for individuals whose neurological arousal patterns have been conditioned by years of evening device use. More invasive interventions, such as brainwave entrainment tech, might be necessary to retrain neural networks that have become adapted to constant stimulation and over-exposure to media mechanisms.
Frequently Asked Questions
Brainwave entrainment uses targeted stimulation to reduce beta activity and enhance alpha (8-13 Hz) and theta (4-8 Hz) production, addressing both symptom categories through unified neurological mechanisms.
This approach explains why Sleep Recovery consistently achieves improvements in both sleep quality and anxiety reduction simultaneously, rather than requiring separate treatments. The precision of modern systems allows targeting of specific neural oscillations that regulate both sleep architecture and anxiety responses.
For treatment approaches, this means that addressing only one condition typically provides incomplete and temporary relief. Treating insomnia without addressing anxiety leaves people vulnerable to stress-related sleep disruption. Treating anxiety without addressing sleep disruption leaves them dealing with fatigue-related anxiety exacerbation.
Integrated approaches specifically target this bidirectionality by addressing shared neurological mechanisms. Rather than breaking the cycle at one point, the intervention modifies underlying bioelectrical patterns that maintain the entire feedback loop.
What role does modern technology play in rising insomnia-anxiety rates among younger populations?
The Global Wellness Institute’s 2025 report shows 40% of Gen Z experiencing anxiety-based insomnia at least three times weekly – a 340% increase since 2015, suggesting modern lifestyle factors significantly contribute to insomnia-anxiety comorbidity.
Platforms like Meta and TikTok specifically design engagement mechanisms that trigger anxiety-related brainwave (EEG) responses. Unpredictable reward signals activate the same pathways involved in anxiety disorders.
Research found that individuals using digital devices within two hours of bedtime show 340% higher rates of both sleep anxiety and delayed sleep onset. The combination of physiological arousal from screens and psychological arousal from social media content creates optimal conditions for insomnia-anxiety comorbidity.
Treatment approaches must take into account these modern factors. Traditional sleep restriction recommendations may be insufficient for individuals whose neurological arousal patterns have been conditioned by years of evening device usage. More interventions, such as brainwave entrainment, may be necessary to retrain neural networks that have become adapted to constant stimulation.
For individual wellness and societal health outcomes, the implications could be transformative.